Medicine and Health
Construction of developmentally inspired periosteum-like tissue for bone regeneration
K. Dai, S. Deng, et al.
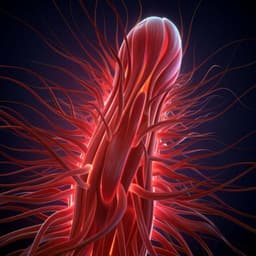
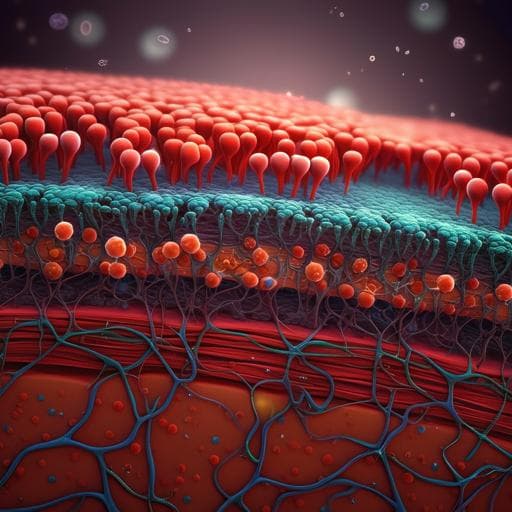
The periosteum covers most bone surfaces and contains diverse cell types (including osteogenic and fibroblastic cells), vasculature, and nerves that collectively orchestrate bone repair and regeneration. Periosteum-derived cells (PDCs) are heterogeneous, include multipotent subpopulations (e.g., LepR+ mesenchymal stromal cells), and contribute to bone, cartilage, and marrow formation. Functional periosteal vasculature, notably type H (CD31hiEmcnhi) vessels, couples angiogenesis and osteogenesis. Harnessing the periosteum’s intrinsic regenerative capacity has inspired periosteum-like tissue (PT) engineering for repairing critical-sized defects. Current strategies such as the induced membrane technique require long incubation and complex procedures, while synthetic membranes with or without exogenous cells may have limited regenerative capacity and higher manipulation requirements. Observations that BMP-2 can induce heterotopic ossification rich in recruited stromal cells and type H vessels led to the hypothesis that BMP-2 can directly activate an individual’s endogenous regenerative capacity to construct vascularized, stromal cell-rich PT in vivo. The study aims to create developmentally inspired PT by subcutaneous implantation of BMP-2-loaded scaffolds to initiate endochondral ossification, characterize the resulting PTs (cells, vasculature, function), and test whether adding chondroitin sulfate (CS) can further enhance PTDC recruitment and function and improve bone regeneration in transplantation assays, including in aged mice.
Background literature highlights the periosteum as a key contributor to fracture repair and bone remodeling, harboring PDCs and functional vasculature (including type H vessels) that couple angiogenesis and osteogenesis. LepR+ cells represent major adult bone marrow MSCs and are present in periosteum as a critical PDC subset. Prior periosteum-mimetic approaches include the induced membrane (Masquelet) technique (effective but slow and surgically complex) and synthetic or biological membranes sometimes seeded with exogenous cells (which increase manipulation and cost). Studies showed human periosteal cell-loaded scaffolds induce ectopic bone formation, and BMP-2 can drive heterotopic ossification with abundant stromal cell recruitment and type H vessels. Glycosaminoglycans such as chondroitin sulfate can modulate BMP-2 stability and osteogenic activity and bind calcium ions, potentially enhancing mineralization. TRAP+ macrophage-lineage cells can promote type H vessel formation via PDGF-BB and recruit PDCs. Aging impairs PDC function and vascular niches, complicating repair of critical-sized defects. These findings motivate a cell-free, in vivo strategy leveraging BMP-2-driven endochondral ossification and matrix components (e.g., CS) to generate functional, vascularized PTs for bone repair.
Study design: Cell-free, in vivo construction of periosteum-like tissue (PT) by subcutaneous implantation of gelatin scaffolds loaded with BMP-2 with or without chondroitin sulfate (CS), followed by characterization of induced PTs and evaluation in allogenic and autologous transplantation models in mice, including aged cohorts. Scaffold fabrication: Porous absorbable gelatin sponges (5 mm diameter × 5 mm thickness; Jiangxi Xiangen, China) were loaded with one of: PBS (60 μL); rhBMP-2 (30 μg in 60 μL); or rhBMP-2 (30 μg) plus CS (30 μg) in 60 μL. Scaffolds were freeze-dried and stored at −20 °C. Scaffold microstructure assessed by FE-SEM. Animals: Male C57BL/6 mice (8–10 weeks and 52–56 weeks) and Lepr-Cre; tdTomato mice (C57BL/6 background). Procedures approved by institutional IACUC. PT induction: Mice were anesthetized; PBS-, BMP-, or BMP/CS-loaded scaffolds were implanted subcutaneously on the back. After 7 days, induced tissues were explanted for analyses or transplantation. Analyses of PTs: Histology (H&E, Safranin O/Fast Green, TRAP) and immunofluorescence (IF) for periostin, CD31, endomucin (EMCN), Aggrecan, and Osterix. Flow cytometry of PT single-cell suspensions for PTDCs and endothelial subsets. Gating: live CD45−Ter119−CD31− cells to define mesenchymal compartment; undifferentiated PTDCs defined as CD45−Ter119−CD31−CD140a+CD105+ and Lepr-tdTomato+. Endothelial analyses included total ECs (CD45−Ter119−CD31+Sca-1+), arteriolar ECs (CD45−Ter119−CD31hiSca-1hi), and type H (CD45−Ter119−CD31+EMCN+). CFU-F assay performed with 1×10^4 digested cells/well; colonies counted at day 8 (toluidine blue). Gene expression by qPCR on first-passage PTDCs (markers: Sox9, Acan, Runx2, OPN, CXCL12, SCF; normalized to Gapdh). Transplantation assays:
- Allogenic transplantation (PTDC fate): PTs induced in Lepr-Cre; tdTomato donors (PBS, BMP, BMP/CS) were engraved to 5 mm discs and placed onto 5 mm critical-sized calvarial defects in wild-type mice. Evaluations at weeks 3 and 6: histology (H&E, TRAP), IF for type H vessels (CD31+EMCN+), Osterix, and donor-derived LepR+ cells; in vivo IVIS fluorescence/CT imaging at week 6.
- Autologous transplantation (regeneration efficacy): In separate cohorts (8–10 weeks and 52–56 weeks), PTs induced subcutaneously were transplanted into 5 mm calvarial defects in the same mouse. Outcomes at weeks 3 and 6 (young) or week 6 (old): micro-CT (Skyscan 1272; 60 kV, 160 μA, 9 μm voxel) for BV/TV and BMD; histology and IF (type H vessels and Osterix); new bone thickness and osseointegration assessed. Imaging and staining: IF sections stained with primary antibodies (Abcam: CD31, Aggrecan, Osterix, periostin; Santa Cruz: EMCN) and Alexa Fluor-conjugated secondaries; DAPI nuclear counterstain. Confocal imaging (Leica SP8). Flow cytometry on CytoFlex LX or BD Symphony A5; analysis in FlowJo or CytExpert. Statistics: Mean ± SD; two-tailed unpaired t test for two groups; one-way ANOVA with Tukey’s post hoc or two-way ANOVA with Bonferroni post hoc for multiple comparisons. Significance: P < 0.05, < 0.01, < 0.001.
- BMP-2 is indispensable for inducing periosteum-like tissues (PTs) in vivo. BMP and BMP/CS scaffolds generated thick, compact fibrous tissues with periosteum-like architecture, mesenchymal condensation, embedded chondrocytes (Safranin O+), TRAP+ cells, and abundant periostin, LepR+ progenitors, Osterix+ osteoprogenitors, and Aggrecan+ chondrocytes. PBS scaffolds produced thinner granulation tissue with minimal periostin and no osteo/chondroprogenitors.
- PTDC abundance and function: Flow cytometry showed higher LepR+ fractions in BMP (14.53% ± 2.57%) and BMP/CS (19.83% ± 4.49%) vs PBS (6.12% ± 2.92%). Undifferentiated PTDCs (CD45−Ter119−CD31−CD140a+CD105+; LepR-tdTomato+) were higher in BMP/CS than BMP (2.24% ± 0.29% vs 1.41% ± 0.21%); PBS had the highest undifferentiated fraction, consistent with limited differentiation.
- Self-renewal: CFU-F per 1×10^4 cells was higher in BMP/CS vs BMP (57.00 ± 5.30 vs 45.17 ± 3.77); PBS highest (64.17% ± 8.78%).
- Gene expression in PTDCs: BMP/CS increased chondrogenic Acan 1.91× vs BMP; Sox9 similar to BMP but both Sox9 and Acan were higher vs PBS (1.98× and 6.51×, respectively). Osteogenic genes Runx2 and OPN were elevated in BMP and BMP/CS vs PBS, with BMP/CS highest among groups. Stem cell maintenance genes CXCL12 and SCF were markedly higher in BMP/CS vs PBS (20.36× and 10.54×) and vs BMP (4.14× and 2.97×), suggesting enhanced recruitment/maintenance capacity.
- Vascularization and progenitors in PTs: Total ECs were ~2.33% ± 1.26% (PBS), 3.85% ± 1.90% (BMP), 3.69% ± 1.73% (BMP/CS). Arteriolar ECs (CD31hiSca-1hi) were 0.33% ± 0.15% (PBS) vs 2.62% ± 1.34% (BMP) and 2.60% ± 1.04% (BMP/CS). Type H ECs were 0.35% ± 0.15% (PBS) vs 2.66% ± 1.38% (BMP) and 2.64% ± 1.05% (BMP/CS). IF confirmed abundant type H vessels and numerous Osterix+ osteoprogenitors and Aggrecan+ chondroprogenitors in BMP and BMP/CS groups; CS further increased osteo/chondroprogenitor numbers.
- Allogenic transplantation: Transplanted PTs from BMP and BMP/CS groups generated new bone by week 3 with active remodeling (more TRAP+ cells vs PBS). Donor LepR+ PTDCs survived long-term and differentiated into Osterix+ osteoprogenitors within new bone. BMP/CS showed higher numbers and fractions of LepR+Osterix+ osteoprogenitors than BMP; none detected in PBS.
- Autologous transplantation (young mice): At week 6, BV/TV was significantly higher in BMP/CS vs BMP and PBS; BMD increased in BMP and BMP/CS vs PBS without significant difference between BMP and BMP/CS. Histology/IF showed enhanced osteogenesis and vascularized new bone in BMP and BMP/CS; BMP/CS exhibited stronger osseointegration and more Osterix+ osteoprogenitors.
- Autologous transplantation (old mice): At week 6, BMP and BMP/CS PTs repaired larger defect areas vs PBS; BV/TV and BMD were highest in BMP/CS. Histology showed complete integration of new bone with host bone in BMP/CS, partial in BMP, minimal in PBS. New bone was highly vascularized and rich in Osterix+ cells.
- Mechanistic insights: CS likely enhances BMP-2 bioactivity/stability and increases CXCL12 and SCF expression in PTDCs, promoting recruitment and maintenance of regenerative progenitors, thereby increasing osteogenic volume and osseointegration.
The study demonstrates that a developmentally inspired, cell-free strategy using BMP-2-loaded scaffolds can induce periosteum-like tissues in vivo via endochondral ossification, recapitulating key features of native periosteum: compact fibrous architecture, abundant functional vasculature (type H and arteriolar vessels), and skeletal progenitors (LepR+ PTDCs, Osterix+ osteoprogenitors, Aggrecan+ chondroprogenitors). These PTs actively contribute to bone formation and remodeling upon transplantation into critical-sized calvarial defects. Adding chondroitin sulfate further enhances PTDC abundance and function, upregulates CXCL12 and SCF (supporting progenitor recruitment and stem cell maintenance), and increases osteochondral progenitors within PTs, translating to greater osteogenic volume and improved osseointegration, including in aged mice where regeneration is typically impaired. TRAP+ macrophage-lineage cells within PTs may promote vascularization (via PDGF-BB) and progenitor recruitment, aligning with the observed coupling of angiogenesis and osteogenesis. Importantly, the use of clinically familiar, FDA-approved gelatin sponges with BMP-2 supports translational potential compared with more complex cell-seeded constructs. Together, the findings validate the hypothesis that BMP-2-initiated endochondral ossification can activate endogenous regenerative capacity to construct functional PTs, and that ECM components like CS can tune PT performance.
This work establishes a cell-free, in vivo method to construct periosteum-like tissue by subcutaneously implanting BMP-2-loaded gelatin scaffolds to trigger endochondral ossification. The induced PTs recapitulate native periosteal architecture, are highly vascularized, and harbor abundant functional PTDCs and osteochondral progenitors that drive bone regeneration and osseointegration in critical-sized cranial defects. Chondroitin sulfate serves as an effective enhancer, increasing PTDC recruitment and osteo/chondroprogenitor abundance and improving regenerative outcomes in both young and aged mice. The approach’s reliance on clinically used materials and growth factors favors translational feasibility. Future work should optimize BMP-2/CS dosing and timing, delineate the cellular origins and mechanisms underlying CS’s effects, and evaluate additional glycosaminoglycans (e.g., keratan sulfate, dermatan sulfate, hyaluronan) for BMP stabilization and mineralization support.
The optimal incubation time and dosing for BMP-2 and CS to fabricate PTs were not fully optimized and require further study. The precise cellular and molecular mechanisms by which CS enhances PTDC recruitment and differentiation remain to be elucidated. The lineage origin of PTDCs within induced PTs was not comprehensively dissected and will benefit from additional lineage-tracing studies. Findings are derived from murine subcutaneous induction and cranial defect models; translation to large animal models and clinical settings remains to be validated.
Related Publications
Explore these studies to deepen your understanding of the subject.