Veterinary Science
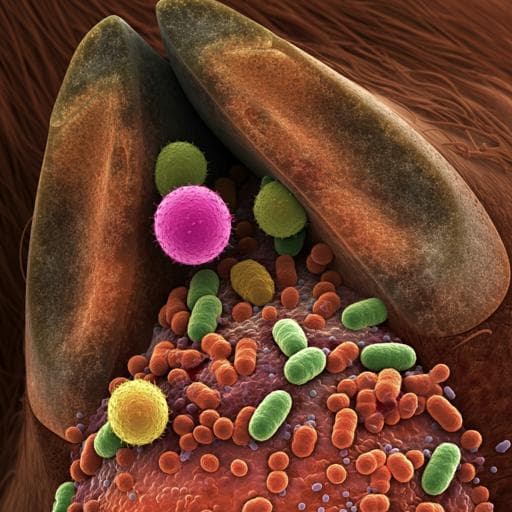
Virulence-determinants and antibiotic-resistance genes of MDR- *E. coli* isolated from secondary infections following FMD-outbreak in cattle
A. M. Algammal, H. F. Hetta, et al.
This groundbreaking study explores the prevalence and antibiotic resistance of *E. coli* in cattle post-foot-and-mouth disease outbreak in Egypt. The authors reveal alarming multidrug resistance patterns and significant virulence genes, presenting a critical public health concern. With 100% prevalence of the *phoA* gene and promising treatments identified, this research by Abdelazeem M. Algammal and colleagues sheds light on an urgent issue facing livestock health.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.