Medicine and Health
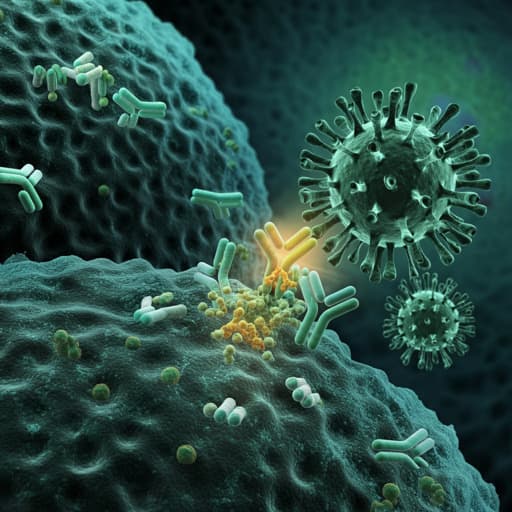
Review on the Safety and Efficacy of COVID-19 Vaccines Approved in Saudi Arabia
T. A. Alhandod, S. I. Rabbani, et al.
This systematic review delves into the safety and efficacy of four COVID-19 vaccines approved in Saudi Arabia, revealing crucial insights on local and systemic reactions, as well as highlighting the need for caution in specific populations. Conducted by Thekra Ali Alhandod, Syed Imam Rabbani, Mansour Almuqbil, Syed Arif Hussain, Nasser Fawzan Alomar, Manzoor Ahmad Mir, and Syed Mohammed Basheeruddin Asdaq, this research is a significant contribution to vaccine safety knowledge.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.







