Medicine and Health
Neutralizing IFNγ Improves Safety without Compromising Efficacy of CAR-T Cell Therapy in B-cell Malignancies
S. Manni, F. D. Bufalo, et al.
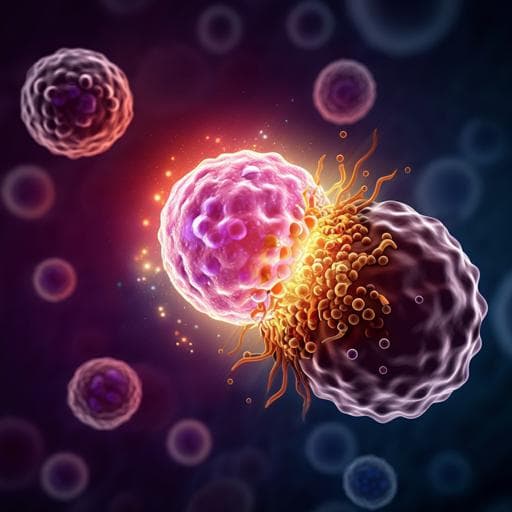
The study addresses whether neutralizing interferon-gamma (IFNγ) can improve the safety of CAR-T cell therapy for B-cell malignancies without diminishing antitumor efficacy. CAR-T therapy is effective but limited by toxicities such as cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), and HLH/MAS, which range from mild to life-threatening. ICANS and CRS share a hyperinflammatory pathophysiology with high cytokine levels; IFNγ is prominently elevated after CAR-T engagement and can activate monocytes/macrophages, amplifying release of IL-6, IL-10 and other mediators, and promoting endothelial activation and blood-brain barrier disruption. Current treatments like corticosteroids can impair CAR-T persistence and efficacy, while tocilizumab (IL-6R blockade) mitigates CRS but is ineffective against ICANS and may worsen neurotoxicity due to poor CNS penetration and altered cytokine trafficking. Pericyte responses to IFNγ and downstream endothelial activation implicate IFNγ as a driver of neurotoxicity. Therefore, the authors test emapalumab, an FDA-approved anti-IFNγ monoclonal antibody for primary HLH, as a strategy to blunt CAR-T–associated toxicities. They hypothesize that IFNγ neutralization will reduce CRS/HLH/MAS and brain injury without compromising CAR.CD19-T antitumor activity.
The paper situates its research within: (a) the high incidence of CRS (30–100%, with 10–30% severe) and ICANS (noted across lymphomas and B-ALL) after CAR-T therapy; (b) evidence that IFNγ surges post-CAR engagement activate macrophages/monocytes and endothelial cells, increasing BBB permeability and contributing to neurotoxicity; (c) limitations of current management: steroids can blunt CAR-T efficacy; tocilizumab reduces CRS but not HLH/MAS or ICANS and may increase severe ICANS when used prophylactically due to CNS cytokine dynamics; (d) recent guideline recommendations to use corticosteroids for grade 2–3 ICANS; (e) the clinical availability and favorable safety profile of emapalumab for primary HLH; and (f) preclinical/clinical observations supporting IFNγ pathway inhibition as a means to decrease macrophage activation and hyperinflammation. These works collectively motivate testing IFNγ neutralization during CAR-T therapy.
- In vitro cytotoxicity: Peripheral blood mononuclear cells (healthy donors) were transduced with a 4-1BB-based CAR.CD19 construct (FMC63 scFv, CD34 epitope tag, CD8 hinge, CD3 transmembrane, 4-1BB and CD3ζ endodomains). CD28-based CAR.CD19 was also tested. CAR-T or non-transduced (NT) T cells were co-cultured with CD19+ Burkitt lymphoma cell lines (Daudi GFP+, Raji FF-Luc) at various effector:target ratios with emapalumab 0–100 µg/mL. Cytotoxicity was assessed via flow cytometry (GFP loss), live-cell imaging (IncuCyte, 64 h kinetics), and short-term (6 h) luciferase assays. Proliferation (CellTrace) and apoptosis assays were performed.
- Activation and gene expression: CAR-T and NT-T cells were activated with recombinant human CD19 Fc chimera (0.5 µg/mL, 16 h). Transcriptional profiling used NanoString panels: 780-gene CAR-T Characterization Panel and, for brain sections, a 770-gene Human Glial Profiling Panel. Differential expression analyses used NanoString Advanced Analysis (p<0.05), with enrichment via Enrichr and network analysis via STRING.
- Cytokine/chemokine measurements: IFNγ, Granzyme B, IL-2, TNF-α, IL-6, IL-8, CXCL9/MIG, CXCL10/IP-10 quantified using the ELLA immunoassay system from 24 h co-cultures and mouse peripheral blood.
- In vivo efficacy (NSG model): Female NOG/NSG mice were engrafted i.v. with 0.25×10^6 Daudi FF-Luc (day −2 or day −8 depending on setting). Mice received NT or CAR.CD19 T cells (10×10^6) and were treated with vehicle or emapalumab 100 mg/kg intraperitoneally on defined schedules (e.g., days 7,11,15 in low tumor burden; earlier dosing in high burden). Tumor burden was monitored by IVIS bioluminescence.
- Humanized CRS/neurotoxicity model: hGM-CSF/hIL-3 NOG mice were humanized with cord blood CD34+ HSCs (≥25% human CD45+ required). Mice were infused with irradiated (sublethal) Daudi FF-Luc cells and then CAR.CD19 T cells to provoke severe toxicity. Emapalumab 100 mg/kg/day or vehicle was given on days 3 and 4 post T-cell infusion. Survival (Kaplan–Meier), serum cytokines (Day 3 and 4), and brain pathology (H&E; quantification of hemorrhagic area) were assessed. Brain tissues underwent NanoString glial panel profiling to identify pathways modulated by IFNγ neutralization. Bone marrow histology assessed phagocytic activity/mitoses.
- Statistics: Data are mean±SD; Student’s t-test or Mann–Whitney for group comparisons (two-sided, p<0.05 significant). Kaplan–Meier with log-rank test for survival. Sample size planning aimed to detect differences of 2 SD at α=0.05 with 80% power. Replicates: in vitro experiments with at least three HD donors; animal cohorts typically n=4 per group in efficacy studies, with pooled samples in some cytokine analyses.
- In vitro efficacy preserved: Across long-term co-cultures and real-time cytotoxicity assays, emapalumab (0–100 µg/mL) did not impair CAR.CD19 T-cell killing of Daudi or Raji targets, nor did it alter CAR-T proliferation. Early (6 h) luciferase-based killing was also unchanged. CD28- and 4-1BB–based CARs showed similar results.
- CAR-T activation/transcriptional effects: Upon antigen stimulation, CAR-T cells exhibited expected activation-associated gene changes vs NT cells. The addition of emapalumab modestly altered expression (14 genes differentially expressed), without indicating suppression of activation signaling pathways relevant to function.
- NSG antitumor activity retained: In low tumor burden models, CAR.CD19 T cells controlled lymphoma comparably with or without emapalumab; no significant difference in bioluminescence at endpoint (e.g., day 28 p=0.58). In higher tumor burden or varied dosing settings, cohorts receiving emapalumab maintained significant tumor control, including in a cohort receiving 1×10^6 CAR-T cells (Supplementary data), indicating emapalumab did not diminish efficacy.
- Humanized CRS model—cytokine modulation and survival: Emapalumab led to complete neutralization of circulating IFNγ and significantly reduced downstream inflammatory mediators. Notably, CXCL9 (MIG) decreased (Day 3 p=0.007; Day 4 p<0.001), CXCL10 (IP-10) decreased (Day 3 p=0.002; Day 4 p=0.005), and human IL-6 levels were significantly reduced versus vehicle. Survival improved dramatically: all emapalumab-treated mice survived the entire 15-day observation, whereas vehicle-treated mice died within 7 days after CAR-T infusion.
- Neuroprotection: Emapalumab significantly reduced brain hemorrhagic areas in mice developing CAR-T–related toxicity, with histology resembling controls without CAR-T cells (p=0.045). Brain transcriptomics revealed 33 significantly deregulated genes (32 downregulated) in emapalumab-treated mice, enriched for oxidative stress, IFN signaling, and chemokine/cytokine-mediated inflammatory pathways, consistent with reduced neuroinflammation.
- HLH/MAS-related pathology: Bone marrow histology from emapalumab-treated mice showed reduced phagocytic cells/mitoses, consistent with mitigation of HLH/MAS-like hyperinflammatory features.
The results support the central hypothesis that IFNγ drives key components of the hyperinflammatory cascade underlying CRS, HLH/MAS, and neurotoxicity after CAR-T infusion. Neutralization of IFNγ with emapalumab blunted systemic cytokine amplification (reduced IL-6, CXCL9, CXCL10), improved survival, and prevented brain hemorrhages in a humanized model that recapitulates severe CAR-T–related toxicities. Importantly, IFNγ blockade did not compromise CAR.CD19 T-cell cytotoxicity or expansion in vitro, nor did it diminish antitumor control in murine xenograft models across tumor burden settings. Transcriptional analyses indicated minimal perturbation of CAR-T activation programs and substantial downregulation of neuroinflammation-associated pathways in brain tissue after emapalumab, aligning mechanistically with the observed protection from brain injury. These findings address clinical needs unmet by current interventions (e.g., tocilizumab’s limitations in ICANS and steroid-related efficacy concerns) and suggest that targeting IFNγ may dissociate efficacy from toxicity, potentially expanding the therapeutic window of CAR-T therapy.
This study introduces and validates a comprehensive humanized mouse model that reproduces severe CAR-T–associated toxicities, including CRS, HLH/MAS-like features, and brain injury. Using this platform, the authors demonstrate that IFNγ neutralization with emapalumab significantly mitigates systemic inflammation, prevents neurotoxicity-associated brain hemorrhages, and improves survival, while preserving the antitumor efficacy of CD19-directed CAR-T cells. These preclinical data provide a rationale for clinical trials testing emapalumab in combination with CAR.CD19 T cells to enhance safety without sacrificing efficacy. Future research should define optimal timing/dosing relative to CAR-T infusion, assess biomarker-guided initiation (e.g., CXCL9/10 levels), and evaluate generalizability across CAR constructs and targets, as well as longer-term effects on CAR-T persistence and tumor control.
- Preclinical design: Findings are based on xenograft and humanized mouse models; translation to human patients requires clinical validation.
- Sample sizes and pooling: Several in vivo cohorts were small (e.g., n=4 per group), and some cytokine measurements were performed on pooled biological material, potentially limiting resolution and statistical power.
- Short observation window: The humanized toxicity model follow-up extended to 15 days; long-term impacts on CAR-T persistence, memory formation, and late toxicities were not assessed.
- Model specificity: While the humanized model recapitulates key features of CRS/ICANS, species differences, conditioning (irradiated tumor cells), and the specific CAR and tumor models may limit generalizability to all clinical contexts.
Related Publications
Explore these studies to deepen your understanding of the subject.