Biology
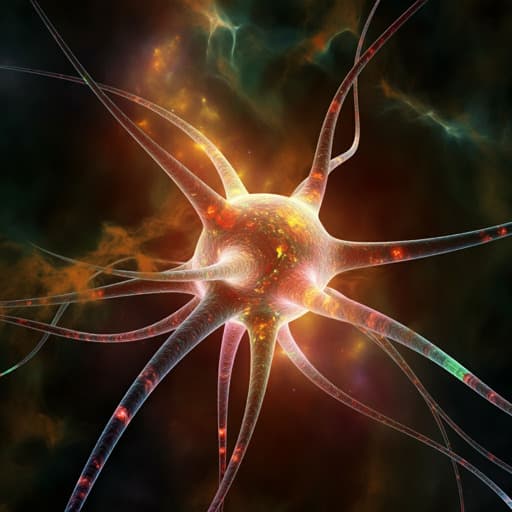
Long-term effects of SARS-CoV-2 infection on human brain and memory
Q. Ding and H. Zhao
Discover the intriguing neurological effects of SARS-CoV-2 as examined by Qiulu Ding and Hanjun Zhao. This review delves into how the virus infiltrates the brain, impacts memory, and the role of various biological factors in long COVID. Learn about potential strategies to mitigate these effects.
Related Publications
Explore these studies to deepen your understanding of the subject.







