Medicine and Health
Injectable decellularized cartilage matrix hydrogel encapsulating urine-derived stem cells for immunomodulatory and cartilage defect regeneration
J. Zeng, L. Huang, et al.
Articular cartilage defects from injury or degeneration are difficult to repair due to the avascular, aneural nature of cartilage and its complex mechanical demands. Current treatments (auto/allografts, biomaterial scaffolds, stem cells) face challenges such as donor site morbidity, low cell survival, and fibrocartilage formation. Human urine-derived stem cells (USCs) offer minimally invasive sourcing, robust proliferation, and multipotent differentiation, showing chondrogenic marker expression in 3D culture, but their application in cartilage engineering remains limited and requires in vivo validation. Biomaterials for cartilage repair include synthetic polymers (e.g., PEG, PCL, PLA) with tunable mechanics but limited biointegration, and natural materials (e.g., chitosan, collagen, gelatin, fibrin) that better support cell function but can elicit immune responses. Decellularized extracellular matrix (dECM) retains native bioactive cues with reduced immunogenicity and has promoted MSC adhesion, proliferation, and chondrogenesis. Processing dECM into injectable hydrogels preserves bioactivity and enables in situ gelation to conform to defect geometry. Given the importance of macrophage-mediated immune responses (pro-inflammatory M1 vs anti-inflammatory, pro-regenerative M2), the study aims to develop an injectable pig cartilage-derived dECM hydrogel encapsulating USCs, evaluate its biocompatibility, chondrogenic induction, and immunomodulatory capacity in vitro and in vivo, and assess cartilage repair in a rat full-thickness defect model.
The study situates itself within prior work using MSCs from adipose tissue, bone marrow, and synovium for chondrogenic repair, noting limitations in invasiveness, proliferation, and phenotype maintenance. USCs have demonstrated chondrogenic potential (GAGs, SOX9, COL-II, aggrecan) after 3D culture, and USC-hyaluronic acid constructs improved neocartilage in rabbits, but broader USC applications remain scarce. Natural vs synthetic biomaterials are contrasted regarding bioactivity and host response. Decellularized matrices retain ECM components while minimizing immunogenic cells; decellularized bovine and pig cartilage scaffolds have supported MSC chondrogenesis and cartilage restoration in animal models. Emerging evidence suggests dECM hydrogels maintain native bioactivity and are injectable. Immunomodulatory properties of decellularized materials and stem cells can influence macrophage polarization toward M2, benefiting cartilage regeneration.
Human USCs were isolated from urine of healthy adult male donors with ethics approval. Urine samples were centrifuged, pellets washed with PBS, and cells cultured in mixed keratinocyte serum-free medium and DMEM-HG with supplements (EGF, bovine pituitary extract, hydrocortisone, transferrin, insulin, adenine, T3) at 37°C, 5% CO2. Passage 3 USCs were used. Proliferation was assessed by CCK-8 and CyQUANT assays. Flow cytometry profiled surface markers (positive: CD73, CD105, CD29, CD44, CD90; negative: HLA-DR, CD19, CD34, CD45). Multilineage differentiation: osteogenesis (ALP, Alizarin Red), adipogenesis (Oil Red O), and chondrogenesis by 3D pellet culture for 28 days with histology (H&E, Alcian blue, Safranin O), immunohistochemistry (COL-II, aggrecan), and RT-qPCR (COL-II, ACAN, SOX9). Pig articular cartilage was decellularized: lyophilization, pulverization, detergent (1% Triton X-100 in Tris-HCl pH 8.0), DNase I and RNase digestion, trypsin-EDTA treatment, washing, freezing, and lyophilization. The decellularized ECM (ECM powder) was solubilized in 0.1 M HCl with pepsin (1 mg/mL) at 4°C for 2 days, neutralized with NaOH at 4°C to physiological pH, then incubated at 37°C to form hydrogels at different concentrations (10–40 mg/mL). Gelation time was measured by tube inversion. Characterization included DAPI/H&E for decellularization efficacy; biochemical assays for DNA (Picogreen), GAG (Blyscan), collagen (hydroxyproline); SEM for microstructure; swelling studies in PBS; FT-IR spectroscopy; and rheology (G′, G″ vs temperature, 0.159 Hz). Biocompatibility was tested by encapsulating USCs in dECM pre-gel and gelating at 37°C; cell viability (Live/Dead), proliferation (CCK-8), and morphology/attachment (SEM) were evaluated over 3–14 days. In vitro chondrogenic capacity was tested by culturing USC-laden hydrogels for 28 days in standard medium or chondrogenic medium (ascorbic acid, TGF-β3, dexamethasone, proline, sodium pyruvate, ITS), followed by histology (H&E, Alcian blue), biochemical quantification of GAG and COL-II, and RT-qPCR (ACAN, SOX9, COL-II). Immunomodulatory effects were assessed in vitro using RAW264.7 macrophages in Transwells: control (M0 in standard medium), M1 positive control (100 ng/mL LPS + 20 ng/mL IFN-γ), M2 positive control (20 ng/mL IL-4), dECM hydrogel (30 mg/mL in upper chamber), and pepsin control. After 48 h, morphology (bright-field, phalloidin/DAPI), immunofluorescence for iNOS (M1) and CD206 (M2), flow cytometry for CD86 and CD206, and RT-qPCR for iNOS, TNF-α, ARG-1, CD206 were performed. In vivo immunomodulation: subcutaneous injection of 0.4 mL dECM hydrogel into SD rats, with explant analysis at days 7 and 14 by gross observation, H&E, and immunohistochemistry (CD86, CD206). Cartilage repair model: 12-week-old male SD rats received full-thickness trochlear cartilage defects (2 mm diameter, 0.5 mm depth). Groups: sham, untreated defect, USCs only (1×10^6 cells/50 µL), dECM hydrogel only (50 µL, 30 mg/mL), and USC-laden dECM hydrogel (1×10^6 cells in 50 µL dECM). Animals were sacrificed at 6 and 12 weeks. Outcomes: gross appearance, histology (H&E, Safranin O/Fast Green, Toluidine Blue), immunohistochemistry (aggrecan, COL-I, COL-II) with ImageJ quantification, and ICRS visual histological scoring by blinded evaluators. Statistics: one-way ANOVA with Tukey post hoc; P<0.05 significant.
- USCs were successfully isolated, clonogenic, and proliferative: by CyQUANT, cell numbers increased ~40.93-fold by day 3, ~65.68-fold by day 5, and ~71.82-fold by day 7 vs day 1. They expressed MSC markers (CD73, CD105, CD29, CD44, CD90) and lacked hematopoietic markers (HLA-DR, CD19, CD34, CD45). They showed osteogenic/adipogenic differentiation and robust chondrogenesis in 3D pellets with strong Safranin O staining and increased COL-II, ACAN, SOX9 mRNA.
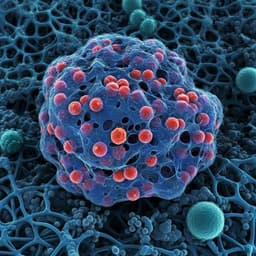
- dECM hydrogel formation and properties: Pre-gels at 4°C gelled at 37°C with gelation times of 14, 9, 3, and 7 min for 10, 20, 30, and 40 mg/mL, respectively. Decellularization markedly reduced DNA to 23.5 ng/mg, with collagen and GAG contents of 259.1 ± 12.45 and 15.38 ± 2.22 ng/mg, indicating collagen retention with partial GAG preservation. Hydrogels had porous architecture (pore size decreased with concentration), high swelling (~1400%), characteristic FT-IR peaks of amide and polysaccharide groups, and a storage modulus reaching 1065.39 ± 113.05 Pa at 37°C (G′ > G″ at physiological temperature).
- Biocompatibility: USC-laden dECM hydrogels supported high viability and proliferation up to day 7; cells displayed spindle/rice-grain morphology and attached well within the matrix.
- In vitro chondrogenesis within dECM: Histology showed chondrocyte-like morphology and lacunae with cartilage-specific matrix (Toluidine blue/Alcian blue). Biochemical assays showed higher GAG and COL-II in chondrogenic vs standard medium (GAG: 16.7 ± 6.5 vs 6.3 ± 7.5, P<0.001; COL-II: 301.0 ± 44.3 vs 131.0 ± 24.6, P<0.05). RT-qPCR showed significant upregulation of ACAN, SOX9, COL-II in chondrogenic medium.
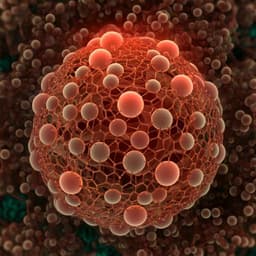
- Immunomodulation in vitro: dECM-treated RAW264.7 cells exhibited M2-like morphology. Immunofluorescence showed reduced iNOS and increased CD206 vs control; pepsin alone had no effect. Flow cytometry indicated elevated CD206 positivity (48.1% and 29.7% in dECM groups) with moderate CD86 (48.8%, 52.5%). RT-qPCR: dECM downregulated pro-inflammatory iNOS and TNF-α and upregulated ARG-1 and CD206, indicating M2 polarization.
- Immunomodulation in vivo (subcutaneous): Day 7 showed more CD86+ macrophages that decreased by day 14, while CD206+ cells increased by day 14, suggesting an initial M1 response transitioning to M2 during remodeling; hydrogels showed smooth encapsulation without granulation and evidence of neovascularization, with gradual degradation by day 14.
- Cartilage repair in rats: USCs-laden dECM hydrogel yielded best gross repair with smooth, integrated hyaline-like cartilage at 12 weeks vs rough, poorly regenerated tissue in untreated defects. Histology (H&E, Safranin O, Toluidine Blue) showed abundant GAG and organized cartilage-subchondral bone interface in the USC+dECM group; USCs-only or dECM-only showed partial improvements. Immunohistochemistry: higher COL-II and aggrecan and lower COL-I in USC+dECM at 6 and 12 weeks vs other groups. ICRS scores (mean ± SD) at 6 weeks: sham 0.2 ± 0.4, defect 8.8 ± 2.3, USCs 5.5 ± 2.2, dECM 5.3 ± 2.6, USC+dECM 4.5 ± 2.0; at 12 weeks: sham 0.3 ± 0.5, defect 7.5 ± 1.9, USCs 4.7 ± 1.6, dECM 3.3 ± 1.2, USC+dECM 2.5 ± 1.0.
The study demonstrates that an injectable pig cartilage-derived dECM hydrogel provides a supportive microenvironment for human USCs, enhancing their survival, proliferation, and chondrogenic differentiation. The hydrogel’s retained ECM components and appropriate mechanics likely supplied native biochemical cues facilitating matrix deposition (COL-II, aggrecan) without requiring extensive exogenous induction. Critically, the dECM hydrogel modulated macrophage responses, attenuating M1-associated inflammatory signaling (iNOS, TNF-α) and promoting M2 polarization (CD206, ARG-1) in vitro and in vivo, which is conducive to tissue remodeling and cartilage regeneration. In a rat full-thickness defect model, the combination of USCs with dECM achieved superior structural and biochemical repair compared to USCs or dECM alone, with increased GAG content, higher COL-II/aggrecan, and reduced COL-I expression, indicating hyaline-like cartilage regeneration and improved integration with subchondral bone. These findings support the dual role of the USC-laden dECM hydrogel as both a chondrogenic and immunomodulatory therapy, addressing key barriers in cartilage repair: cell scarcity, phenotype maintenance, and deleterious inflammation.
An injectable decellularized cartilage matrix hydrogel encapsulating human urine-derived stem cells was developed and shown to be biocompatible, chondrogenic, and immunomodulatory. The hydrogel supported USC viability and promoted cartilage-specific matrix production in vitro, induced favorable macrophage polarization, and significantly enhanced cartilage repair in a rat defect model, yielding hyaline-like, well-integrated neocartilage. These results suggest USC-laden dECM hydrogels are a promising biomaterial strategy for cartilage regeneration. Future work could optimize hydrogel composition and dosing, assess long-term durability and mechanics of regenerated cartilage, and evaluate translational potential in larger animal models.
Related Publications
Explore these studies to deepen your understanding of the subject.