Medicine and Health
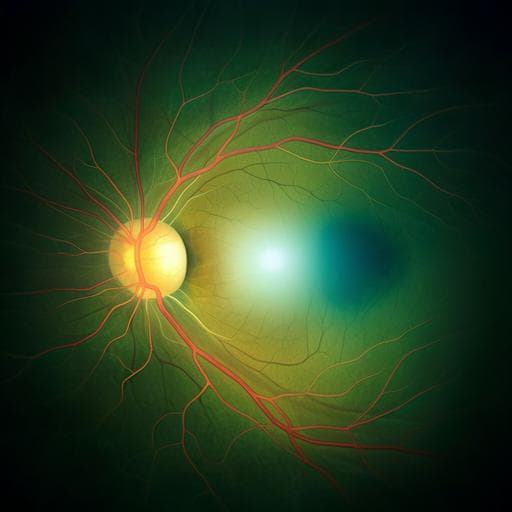
Evaluation of care with intravitreal aflibercept treatment for UK patients with diabetic macular oedema: DRAKO study 24-month real-world outcomes
S. Sivaprasad, F. Ghanchi, et al.
The DRAKO study highlights the effectiveness of standard-of-care intravitreal aflibercept treatment for diabetic macular edema in the UK, showcasing impressive outcomes even with low injection frequencies. Conducted by an expert team of authors, the research reflects real-world clinical practices and maintains high patient quality-of-life scores.
Related Publications
Explore these studies to deepen your understanding of the subject.