Medicine and Health
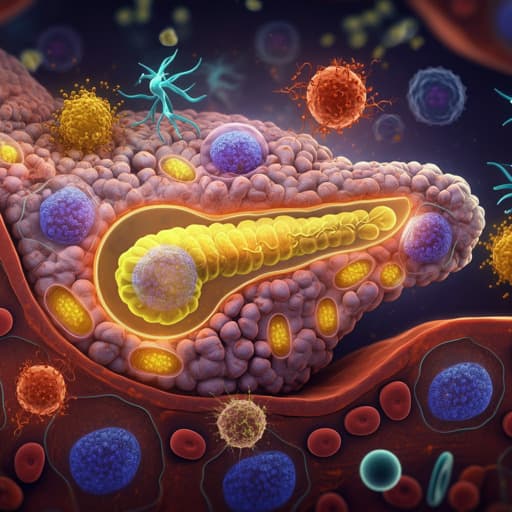
Type I Diabetes Pathoetiology and Pathophysiology: Roles of the Gut Microbiome, Pancreatic Cellular Interactions, and the 'Bystander' Activation of Memory CD8 + T Cells
S. Santillo, Damiano, et al.
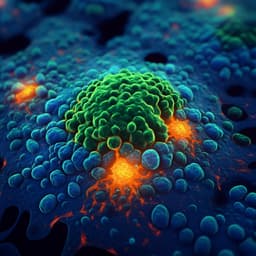
Explore the intricate relationship between mitochondrial melatonin pathways, gut microbiome interactions, and immune responses in Type 1 diabetes mellitus as reviewed by Simona Santillo, Damiano, and George Anderson. Discover how these factors interplay, leading to β-cell apoptosis and autoimmune effects.
Related Publications
Explore these studies to deepen your understanding of the subject.