Medicine and Health
Targeting IL-21 to tumor-reactive T cells enhances memory T cell responses and anti-PD-1 antibody therapy
Y. Li, Y. Cong, et al.
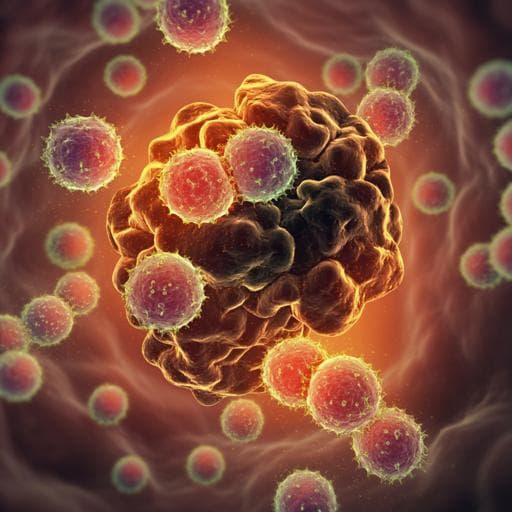
PD-1 blockade can reinvigorate tumor-reactive CD8+ T cells by interrupting PD-1/PD-L1 inhibitory signaling, yet clinical benefit is limited to a minority of patients. Effective responses to PD-1 blockade depend on the presence, reactivation, and proliferation of antigen-experienced CD8+ T cells within the tumor microenvironment. Common γ-chain cytokines (IL-2, IL-15, IL-21) regulate the magnitude and function of CD8+ T cell responses, with IL-21 playing a key role in the development and maintenance of memory CD8+ T cells and acting synergistically with IL-7 to promote proliferation and survival. Tumor-reactive T cells expanded under IL-21 influence display superior antitumor activity, and IL-21 enhances outcomes in adoptive and checkpoint therapies in preclinical models. However, systemic cytokine administration is limited by short half-life, broad activity, and toxicity. Because PD-1 is upregulated on activated and chronically stimulated tumor-specific T cells and marks tumor-reactive TILs, the authors hypothesized that fusing IL-21 to an anti-PD-1 antibody would target IL-21 selectively to PD-1+ tumor-reactive T cells in vivo, enhancing efficacy while reducing off-target effects.
Prior work established that: (1) responses to PD-1 blockade require antigen-experienced CD8+ T cells in the TME; (2) IL-21 promotes early differentiation phenotypes and sustains memory CD8+ T cells, synergizing with IL-7 to support proliferation/survival; (3) IL-21-driven expansion yields tumor-reactive T cells with superior in vivo antitumor activity compared to IL-2/IL-15; (4) ex vivo programming with IL-21 facilitates generation of human memory stem-like T cells (TSCM) and improves adoptive T cell therapies; (5) IL-21 provides key CD4+ T cell help to boost CD8+ responses and enhances anti-CTLA-4 and anti-PD-1 efficacy in preclinical models. Conversely, systemic cytokine therapy suffers from short half-life and systemic toxicity. PD-1 expression identifies activated tumor-reactive T cells and correlates with clinical responses to PD-1 blockade. These observations provided the rationale for targeting IL-21 to PD-1+ T cells to improve therapeutic precision and potency.
Engineering and protein production: A noncovalent homodimeric anti-PD-1 single-chain variable fragment (scFv) diabody was generated with a 5–amino acid linker and fused sequentially to murine IL-21 and a Flag tag to create PD-1Ab21; a control PD-1Ab without IL-21 was also produced. Constructs were cloned into pTT3 (and anti-PD-1 in pTT5 for production) and transiently transfected into 293E cells. Proteins were purified using anti-Flag affinity and analyzed by SDS-PAGE and size-exclusion chromatography (Sephadex 200). Binding/bioactivity assays: Binding of PD-1Ab21 to PD-1+ EG7 cells and activated OT-1 CD8+ T cells, and competition with PD-L1 binding, were assessed by flow cytometry. IL-21 bioactivity was measured via proliferation of BaF3 cells. In vitro T cell differentiation: Naïve OT-1 CD8+ T cells were primed with OVA257–264 peptide; after 2 days of activation, cells were cultured with IL-2, IL-21, PD-1Ab, PD-1Ab+IL-21, or PD-1Ab21. Phenotypic differentiation toward naïve-like/memory subsets was analyzed by CD44 and CD62L expression; sorted CD44hiCD62Lhi cells were cultured with PD-1Ab21 or control to assess conversion to CD44lowCD62Lhigh; CFSE dilution measured proliferation. Polyclonal CD8+ T cells activated with anti-CD3/CD28 were similarly tested. Transcriptomics: RNA-seq was performed on sorted TN, activated CD44hiCD62Llo, PD-1Ab21-generated CD44lowCD62Lhigh, and IL-2/IL-15-differentiated cells. Analyses included PCA, hierarchical clustering, and DESeq2 for differential expression (BH-adjusted p<0.01, FC>2). In vivo models and treatments: - CT26 (Balb/c) and MC38 (C57BL/6) subcutaneous tumors treated with anti-PD-1, PD-1Ab+IL-21, or PD-1Ab21 via intraperitoneal injection (n=5/group). - TUBO (Her2/neu+) tumors treated with anti-Her2/neu alone, with PD-1Ab+IL-21, or with PD-1Ab21; hydrodynamic plasmid delivery was also tested. - B16-OVA model: C57BL/6 mice received 1×10^6 naïve CD90.1 OT-1 cells prior to tumor inoculation, vaccinated intradermally with OVA257–264 peptide plus poly I:C, and treated with anti-PD-1, PD-1Ab+IL-21, or PD-1Ab21. Receptor occupancy and targeting: PD-1 occupancy on OT-1 cells in blood and tumors was assessed at multiple time points after injection of anti-PD-1 or PD-1Ab21. Tumor sections were stained by immunofluorescence for CD8 and Flag to visualize PD-1Ab21 binding in situ. Immunophenotyping: Flow cytometry of lymphoid organs (DLNs, spleen) and tumors assessed frequencies of CD8+ TSCM (e.g., CD62LhiCD44lowCD122+Sca-1+), TCF1 and CD95 expression, and OT-1 frequencies/phenotypes (e.g., CD44/CD62L; KLRG1/CD127 MPEC vs SLEC). Cytokine production (IFN-γ, IL-2) was quantified by ELISA after PMA/ionomycin restimulation. Statistics: Data presented as mean±SEM or SD; unpaired two-tailed t-test, one-way or two-way ANOVA with multiple-comparison corrections; significance defined as p<0.05. Data availability: RNA-seq deposited in GEO GSE160961.
- Successful construction of a PD-1-targeted IL-21 immunocytokine: PD-1Ab21 formed a predominant noncovalent homodimer, bound PD-1 on EG7 and activated OT-1 cells, and blocked PD-L1 binding comparably to anti-PD-1. It retained IL-21 bioactivity (BaF3 proliferation). - Induction of naïve-like/memory phenotypes from activated CD8+ T cells: PD-1Ab21 converted activated CD44hi OT-1 cells into CD44lowCD62Lhigh naïve-like cells; more than half of PD-1Ab21-cultured cells displayed this phenotype, whereas PD-1Ab alone had no such effect. Sorted CD44hiCD62Lhi cells cultured with PD-1Ab21 progressively became CD44lowCD62Lhigh over 3 days and proliferated more (greater CFSE dilution) than controls. - Transcriptomic alignment with memory T cells: PCA and hierarchical clustering placed PD-1Ab21-generated cells with TN/Tcm clusters. PD-1Ab21 and IL-21 conditions upregulated memory-associated genes (e.g., Ly6a/Sca-1, Fas/CD95, Bcl-6, Tcf7/TCF1). PD-1Ab21-differentiated cells expressed higher TCF1 and CD95 protein. - Superior generation of TSCM-like cells: Across doses, PD-1Ab21 was markedly superior to IL-21 in inducing TSCM-like differentiation from activated T cells; IL-21R:Ig inhibited PD-1Ab21 effects, implicating IL-21R signaling and suggesting added benefits from dimerization and PD-1 targeting. - In vivo targeting and persistence: In vaccinated B16-OVA-bearing mice, PD-1 on circulating OT-1 cells was rapidly occupied after PD-1Ab21 or anti-PD-1 dosing; at 24 h PD-1 remained minimally detectable with PD-1Ab21 but not with anti-PD-1, indicating more sustained occupancy. Immunofluorescence showed PD-1Ab21 (Flag-tag) co-localized with CD8+ TILs, unlike recombinant IL-21. - Expansion of TSCM and tumor-specific CD8+ T cells: PD-1Ab21 increased CD8+ TSCM frequencies in spleen and DLNs; phenotyping indicated retention of resident, self-renewing memory OT-1 cells in DLNs (higher CD62Lhi fractions) vs vaccination±anti-PD-1, which showed more effector-like phenotypes. - Antitumor efficacy superior to controls and combinations: In CT26 and MC38 models, PD-1Ab21 significantly inhibited tumor growth more than anti-PD-1 or PD-1Ab+IL-21 combinations (e.g., CT26: p=0.016, 0.0004, 0.0001 across comparisons; MC38: anti-PD-1 vs PD-1Ab21 p=0.045). In TUBO/Her2 models, combining anti-Her2/neu with PD-1Ab21 significantly improved tumor control over anti-Her2/neu alone or with PD-1Ab+IL-21. In vaccination (B16-OVA) settings, PD-1Ab21 markedly enhanced vaccine efficacy; OT-1 frequencies in TILs of PD-1Ab21-treated mice were about two-fold higher than with anti-PD-1 and exceeded 70% of CD8+ TILs. - Functional enhancement: PD-1Ab21-treated T cell subsets produced robust IFN-γ and IL-2 upon stimulation, and vaccination plus PD-1Ab21 increased MPEC-like (CD127hiKLRG1lo) proportions relative to SLEC-like cells, supporting improved memory quality.
Fusing IL-21 to an anti-PD-1 targeting moiety concentrates cytokine signaling to PD-1+ tumor-reactive T cells, directly addressing the challenge of insufficient T cell activation during PD-1 blockade and mitigating systemic cytokine exposure. PD-1Ab21 rapidly binds activated tumor-specific CD8+ T cells in vivo, reprogramming previously activated cells toward a TSCM-like state characterized by CD62LhiCD44low, TCF1+, CD95+, Sca-1+ profiles and enhanced proliferative potential. This targeted approach generates a self-renewing memory pool in DLNs that can sustain effector responses within tumors, as evidenced by increased OT-1 frequencies (up to >70% of CD8+ TILs) and improved tumor control. Mechanistically, the data support active proliferation-associated differentiation into TSCM rather than the inhibition of differentiation via Wnt signaling pathways, and the dependence on IL-21R signaling was confirmed by IL-21R:Ig blockade. Functionally, PD-1Ab21 outperformed both anti-PD-1 alone and the simple co-administration of IL-21 with anti-PD-1, suggesting that spatially targeted cytokine delivery and possible avidity/dimerization effects are critical for efficacy. The approach synergized with antigen-priming strategies (vaccination, anti-Her2/neu), indicating broad applicability as a combinatorial immunotherapy to augment checkpoint blockade.
This study introduces PD-1Ab21, an anti-PD-1–IL-21 fusion immunocytokine that targets IL-21 to PD-1+ tumor-reactive T cells, promoting rapid generation of memory stem-like CD8+ T cells and enhancing antitumor immunity. PD-1Ab21 demonstrated superior expansion of tumor-specific memory and effector CD8+ T cells and improved tumor control compared with anti-PD-1 alone or with exogenous IL-21. The findings provide a strategy to improve checkpoint blockade efficacy by directing cytokine signaling to the appropriate T cell subset in vivo. Future work should translate this concept using a full-length human anti-PD-1–IL-21 fusion with extended half-life, evaluate safety and pharmacokinetics, and explore combinations with T cell-priming modalities (vaccines, targeted antibodies) across diverse tumor types.
- Preclinical scope: Results are limited to murine models (CT26, MC38, TUBO, B16-OVA) and transgenic TCR systems (OT-1), which may not fully recapitulate human tumor immunobiology. - Pharmacokinetics: The scFv/diabody format likely has a short half-life; in vivo exposure and dosing optimization for a clinical analogue (full-length human IgG fusion) were not addressed. - Safety/toxicity: Systemic safety, cytokine-related adverse effects, and off-tumor effects were not comprehensively evaluated. - Comparative breadth: While comparisons to anti-PD-1 and IL-21 co-administration were made, broader benchmarking against other cytokine fusions or alternative targeting strategies was limited. - Nomenclature/inconsistencies: Some textual inconsistencies (e.g., PD-1Ab1 vs PD-1Ab21) could reflect experimental variants but may complicate interpretation; detailed characterization of each variant’s properties is not fully delineated.
Related Publications
Explore these studies to deepen your understanding of the subject.