Medicine and Health
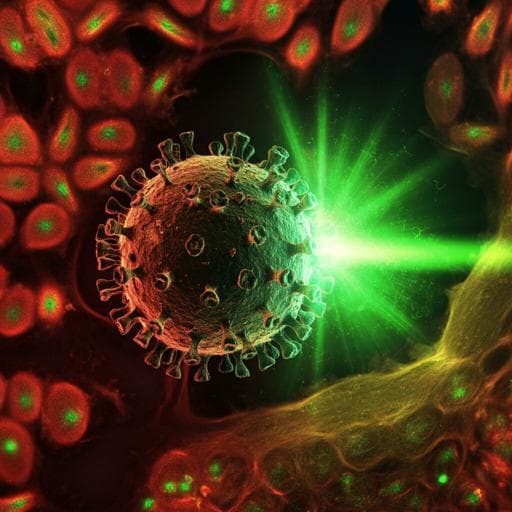
Sulforaphane exhibits antiviral activity against pandemic SARS-CoV-2 and seasonal HCoV-OC43 coronaviruses in vitro and in mice
A. A. Ordonez, C. K. Bullen, et al.
Discover the promising antiviral effects of sulforaphane (SFN), a phytochemical in cruciferous vegetables. This innovative research by Alvaro A. Ordonez and colleagues at Johns Hopkins University showcases SFN's ability to combat SARS-CoV-2 and HCoV-OC43, demonstrating significant reductions in viral load and lung injury in mice. A potential breakthrough in the prevention and treatment of coronavirus infections awaits.
Related Publications
Explore these studies to deepen your understanding of the subject.