Engineering and Technology
Spotlight on Genetic Kidney Diseases: A Call for Drug Delivery and Nanomedicine Solutions
N. Trac, A. Ashraf, et al.
This Perspective addresses the urgent need for targeted drug delivery and nanomedicine solutions for genetic kidney diseases (GKDs), many of which lead to chronic kidney disease (CKD) and end-stage kidney disease (ESKD). The authors contextualize the problem with kidney physiology and disease burden: the kidneys filter ~200 L of blood per day, yet CKD affects ~37 million adults in the US and ~844 million worldwide, with ~800,000 diagnosed with ESKD in the US. Advances in sequencing have linked ~500 monogenic causes to CKD, and 20–30% of pediatric and adult CKD cases have genetic etiologies. Despite nanomedicine’s success in oncology and vaccines, there are no nanotherapies tailored for GKDs. The paper’s purpose is to synthesize kidney-targeted nanomedicine design principles, summarize therapeutic strategies (including for congenital diseases), highlight cell therapy advances, and identify gaps and collaborative actions needed to translate kidney-targeted drug delivery to the clinic.
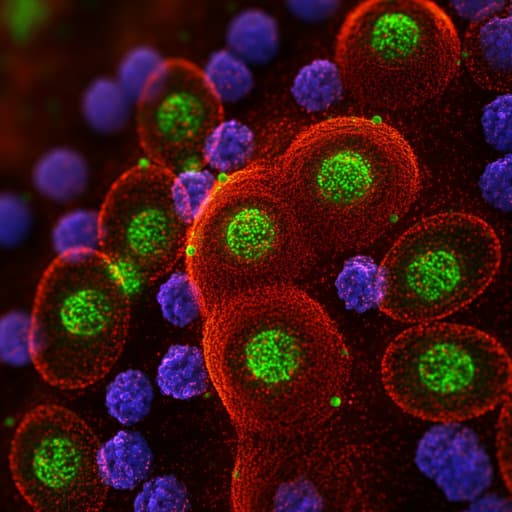
The paper reviews kidney physiology relevant to delivery barriers, focusing on the glomerular filtration barrier (GFB) composed of fenestrated endothelium (50–100 nm fenestrations), glomerular basement membrane (GBM; pores <10 nm), podocyte slit diaphragms (>40 nm exclusion), and the glycocalyx. Literature indicates sub-10 nm particles generally cross the GFB; ultrasmall (<1 nm) particles may be retained in the glycocalyx, with the GFB acting as a band-pass filter (~1–6 nm optimal). Surface charge influences filtration: anionic particles are repelled; cationic and neutral/zwitterionic particles can pass and may avoid protein corona formation. Shape matters: maintaining one dimension <10 nm enables rod-like or cylindrical particles to filter, and non-spherical shapes can extend circulation and increase renal uptake. Under disease, the GFB becomes leakier, increasing renal accumulation of larger particles (e.g., 20 and 100 nm polystyrene showed ~2-fold higher accumulation in glomerular disease models). The review covers strategies to avoid GFB filtration and achieve kidney accumulation via mesangial phagocytosis (~80 nm AuNPs) or basolateral proximal tubule uptake with mesoscale PLGA nanoparticles (350–400 nm) via peritubular capillaries, with retention up to 7 days. Active targeting literature includes peptide ligands (e.g., megalin-targeting (KKEEE)3K, CCD-targeting ELRGDMAAL, glomerulus-targeting CLPVASC), antibodies (e.g., intercalated cell basolateral antibodies; CD163-targeted iron oxide for MRI), and aptamers (RPTEC- and ccRCC-binding sequences). For congenital applications, literature on in utero delivery via vitelline vein and intraamniotic routes shows site-specific biodistribution and durable gene modulation; placental transport studies suggest paracellular channels of 15–25 nm enabling passive passage of <25 nm particles, and active transcytosis supports transport of larger particles (~300 nm cutoff reported). Targeted placental delivery via FcRn (IgG), iRGD, and chondroitin sulfate A ligands is highlighted. Extracellular vesicles engineered for fetal delivery can cross the placenta and enable organ-targeted fetal delivery. Cell therapy literature for GKDs includes stem/progenitor cells in Alport syndrome, BMMSCs in PKD (phase I safety), and renal autologous cell therapy (REACT) trials showing encouraging outcomes. The authors also review emerging computational and machine learning approaches for nanoparticle design, LNP-based nucleic acid therapies (e.g., Onpattro) and organoid models for disease mechanism and drug discovery.
This is a Perspective/narrative synthesis rather than an experimental study. The authors collate and interpret findings from prior clinical, preclinical, and nanomedicine design studies to: (1) outline the clinical landscape and genetic bases of kidney diseases; (2) summarize kidney physiological barriers relevant to nanoparticle delivery; (3) review passive and active nanoparticle targeting strategies and their physicochemical design criteria (size, charge, shape, ligand targeting); (4) survey fetal and placental delivery strategies for congenital kidney diseases; (5) discuss cell-based therapies; and (6) identify translational gaps and propose collaborative and technological pathways (standardized reporting, machine learning, organoid models) to accelerate kidney-targeted therapeutics.
- Disease burden and gaps: CKD affects ~844 million globally and ~37 million in the US; ~800,000 in the US have ESKD requiring dialysis or transplant. Despite nanomedicine success in other fields, no nanotherapeutics are approved or in clinical testing specifically for GKDs. ADPKD affects ~600,000 in the US and ~12.5 million worldwide; tolvaptan (approved 2018) modestly slows cystogenesis but has limited kidney accumulation and safety constraints (REMS). ARPKD is rare (<200,000 affected) with severe perinatal presentation and 20–30% neonatal mortality within 48 hours; there is no cure.
- Kidney delivery design principles: Size is critical for GFB passage: fenestrations 50–100 nm; GBM pores <10 nm; slit diaphragms exclude >40 nm. Particles <10 nm pass; subnanometer particles can be retained in the glycocalyx; the GFB may act as a band-pass filter (~1–6 nm optimal). Charge strongly influences transport: cationic quantum dots (3.5–6.0 nm) appeared in urine at 4 h and showed ~5-fold higher kidney retention vs anionic counterparts at 24 h (15%ID vs 3%ID). Neutral/zwitterionic coatings can reduce opsonization and favor kidney uptake. Shape engineering that preserves one sub-10 nm dimension enables GFB passage of high-aspect-ratio particles and extends circulation time.
- Disease-state permeability: In a glomerular disease mouse model, renal accumulation of 20 and 100 nm nanoparticles increased ~2-fold vs healthy animals, implying altered GFB selectivity under pathology.
- Alternative renal targeting without GFB filtration: ~80 nm gold nanoparticles target mesangial cells via phagocytosis; mesoscale PLGA nanoparticles (350–400 nm) accumulate in kidneys up to 7 days, primarily via basolateral uptake in proximal tubule epithelial cells following transcytosis from peritubular capillaries.
- Active targeting ligands: Peptides such as megalin-targeting (KKEEE)3K (proximal tubule, early PKD), ELRGDMAAL (cortical collecting duct, later PKD and CCD disorders), CLPVASC (glomerulus). Antibodies can target basolateral intercalated cells in CCD and enable diagnostics (e.g., CD163-targeted iron oxide nanoparticles for MRI in AKI). Aptamers identified for RPTECs and ccRCC show selective binding in vitro.
- Congenital delivery strategies: Intraamniotic antisense oligonucleotide delivery reduced MALAT1 3-fold in pups one week post-birth; in utero protein replacement (ectodysplasin-IgG) corrected a congenital phenotype. PLGA nanoparticles via vitelline vein accumulated in fetal liver, whereas intraamniotic delivery targeted fetal lungs and GI; off-target gene delivery was <0.000002%. Ionizable LNP formulation (B-4) showed fetal kidney uptake after vitelline delivery in mice. Placental transport pathways include paracellular channels (15–25 nm; passive for <25 nm) and active transcytosis (cutoff ~300 nm observed in some studies); targeting FcRn with IgG, iRGD for αv integrins, and CSA peptides enhanced placental crossing and fetal effects.
- Cell therapies: Bone marrow-derived progenitors, human chorionic stem cells, and amniotic fluid stem cells benefit Alport syndrome via differentiation and paracrine mechanisms (e.g., EVs reducing VEGF-mediated damage). BMMSCs demonstrated phase I safety in ADPKD; REACT using autologous selected renal tubular cells showed formation of neo-kidney-like tissue and a decline in eGFR slope over 1 year in early data.
- Translational enablers: Standardized nanoparticle formulation and reporting to enable machine learning; organoid and organ-on-chip models for mechanism and screening; leveraging LNP platforms validated clinically (e.g., Onpattro siRNA; mRNA-LNPs in trials for metabolic diseases).
The synthesis underscores that GKDs are prevalent, genetically heterogeneous, and largely untreated at the root-cause level. Existing small molecules (e.g., tolvaptan) are limited by poor kidney accumulation and systemic toxicity. By mapping kidney barriers and summarizing physicochemical rules for nanoparticle transport (size, charge, shape) alongside ligand-based active targeting, the Perspective directly addresses how to rationally design carriers to reach specific nephron segments and cell types. Recognizing that pathological changes can increase GFB permeability suggests disease-tailored designs may further improve delivery. For congenital disease, the review delineates feasible in utero routes (vitelline vein, intraamniotic) and placental-crossing strategies, with supportive data on biodistribution, durability of gene modulation, and safety considerations. Cell therapy findings indicate complementary avenues for tissue regeneration and immunomodulation. Together, these insights set the stage for multi-modal interventions (nanoparticle drug/gene delivery, cell-based therapies) and emphasize the need for validated ligands, disease-relevant models, and standardized datasets to speed translation, thereby aligning the field toward therapies that can intervene earlier and more precisely in GKDs.
This Perspective consolidates the clinical need and provides a roadmap for nanomedicine and cell therapy in genetic and congenital kidney diseases. Key contributions include: (1) defining kidney-specific delivery barriers and practical nanoparticle design principles; (2) highlighting active targeting ligands for distinct nephron regions; (3) outlining fetal and placental delivery strategies for congenital disorders; and (4) summarizing promising cell therapy approaches. The authors call for cross-disciplinary collaboration, standardized nanoformulation and reporting to enable machine learning, expanded ligand discovery (phage display, aptamers, in silico), improved disease models (organoids, organ-on-chip), and leveraging established LNP platforms to accelerate kidney-targeted nucleic acid therapies. Future research should clarify genotype–phenotype relationships, validate targeting ligands in disease contexts, study protein coronas in renal delivery, and determine optimal delivery routes and formulations tailored to specific GKDs and disease stages.
As a Perspective, this work does not present new experimental data but synthesizes existing studies that vary in model systems, nanoparticle chemistries, and endpoints, limiting direct comparability. Many cited findings are preclinical, with scarce data from kidney disease models that reflect human pathology, and virtually no clinical kidney-targeted nanomedicines for GKDs. Ligand repertoires for specific renal cell types remain limited and insufficiently validated in disease settings. For congenital delivery, ethical and regulatory constraints, limited targets for placental transport, and species differences complicate translation; some nanoparticles (e.g., silica, TiO2) have caused pregnancy complications in mice. Overall, gaps in genotype–phenotype knowledge, biomarkers, and robust animal or human-relevant models constrain generalizability and immediate clinical applicability.
Related Publications
Explore these studies to deepen your understanding of the subject.