Medicine and Health
speedingCARs: accelerating the engineering of CAR T cells by signaling domain shuffling and single-cell sequencing
R. Castellanos-rueda, R. B. D. Roberto, et al.
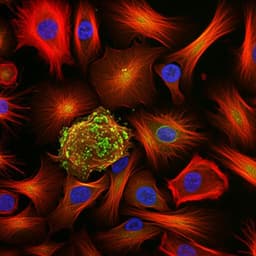
CAR T cell therapies have achieved major success in hematological malignancies but face challenges in solid tumors, including resistance to killing, relapse via antigen escape, limited persistence, and safety concerns such as cytokine release syndrome and neurotoxicity. Conventional CARs use a narrow set of intracellular signaling domains (CD3ζ with CD28 or 4-1BB), limiting the diversity of T cell activation programs. Prior attempts to enhance function often add complexity (e.g., checkpoint inhibitors, cytokine armoring, drug-controllable designs). Advances in single-cell transcriptomics reveal that CAR design strongly shapes transcriptional responses. The research question is whether combinatorial shuffling of natural immune signaling domains, coupled with pooled single-cell functional screening, can rapidly discover CAR variants that elicit diverse, potentially advantageous T cell phenotypes. The study introduces speedingCARs, integrating domain shuffling, CRISPR-Cas9 knock-in to the TRAC locus, and scRNA-seq/scCAR-seq after tumor co-culture to identify functional CAR architectures and benchmark them against clinical standards and tumor-infiltrating lymphocyte (TIL) phenotypes.
The field has explored strategies to overcome immunosuppression (e.g., checkpoint blockade co-administration, cytokine overexpression, drug- or antigen-tunable CARs), but these add therapeutic complexity. Single-cell profiling has shown CAR composition strongly influences T cell transcriptional states. Clinically, most CARs use CD3ζ with CD28 or 4-1BB; few alternative signaling domains have been tested, often individually, due to low-throughput design and assays. Recent pooled screening approaches (e.g., Gordon et al., Goodman et al.) leveraged FACS and amplicon sequencing to identify novel intracellular domains. However, many earlier screens were unidimensional (reporter readouts in cell lines), limiting translatability compared to primary T cell, multi-omic approaches. This study builds on these insights by using pooled scRNA-seq and scCAR-seq in primary T cells to resolve multi-dimensional phenotypes across a large combinatorial signaling domain space.
Design and construction of CAR signaling domain library: The CAR chassis included CD8α signal peptide, trastuzumab-derived scFv (4D5) targeting HER2, two Strep tags (for detection), a CD28 hinge and transmembrane domain, and a truncated CD3ζ fragment with two ITAMs. The CD3ζ domain was segmented to retain a total of three ITAMs in the assembled CARs. Two pools of intracellular domains were created: Domain A (15 co-stimulatory/immune receptor-derived domains, e.g., CD28, 4-1BB, CD30, CD150/SLAM, CD84, FCRL6, CD244, LAG3) and Domain B (12 single-ITAM-containing domains, e.g., FcγRIIa, DAP12, CD79b, CD3G, plus viral proteins LMP2, K1, GP, and the first segment of CD3ζ). Type IIS restriction cloning (AarI) ensured ordered ligation of one A and one B domain, joined by a minimal linker, yielding 180 possible combinations. Library diversity and balance were validated by long-read sequencing (179/180 combinations present).
Primary T cell genome editing and CAR expression: Primary human T cells from healthy donors were isolated, activated with CD3/CD28 beads, and cultured in IL-2–supplemented medium. CRISPR-Cas9 RNPs and HDR templates were used to knock-in the CAR library into the TRAC locus, simultaneously disrupting endogenous TCR. Post-editing, CAR+TCR− cells were enriched by FACS using Strep tag staining and CD3ε negativity. Targeted integration was confirmed by genotyping. HER2 binding was validated by flow cytometry.
Pooled functional screening by scRNA-seq and scCAR-seq: CAR library T cells were co-cultured 36 h with HER2+ SKBR3 tumor cells (E:T 1:2) to activate signaling. Benchmarks (28z, BBz) were spiked-in; negative controls included TCR− T cells and unstimulated 28z T cells. After co-culture, CAR T cells were sorted and processed via 10x Genomics scRNA-seq (3' v3). In parallel, scCAR-seq amplified CAR transcripts from the 10x cDNA using Strep-tag–specific primers, followed by PacBio SMRT sequencing to deconvolve CAR variant identities and link them to single-cell barcodes.
Data processing and clustering: scRNA-seq reads were aligned to GRCh38 (Cell Ranger v3.1.0) and analyzed in Seurat. QC filters: 500<nFeature_RNA<10,000; mitochondrial reads <15%. scCAR-seq assignments annotated cells with a single CAR variant (55% of cells). Batch integration used reciprocal PCA/SCTransform; dimensionality reduction by PCA/UMAP; unsupervised clustering; marker discovery by FindAllMarkers; gene set enrichment by gProfiler2; gene signature scoring by UCell. Pseudo-bulk profiles per variant enabled PCA and marker analyses. Subsampling up to 250 cells/variant and 500/control was repeated 50 times to assess cluster stability (high ARI).
Mapping to TILs: CD8+ CAR T cells were integrated with a published scRNA-seq dataset of CD8+ TILs from NSCLC patients pre/post anti–PD-1 (Liu et al., GSE179994). After QC and SCTransform, datasets were merged and batch corrected with Harmony, then clustered and visualized by UMAP. Enrichment of CAR cells in TIL-associated clusters was assessed.
Functional validation assays: Ten CAR variants (A–J) plus 28z and BBz were selected based on scRNA-seq and TIL mapping. Surface expression/differentiation: 18-marker flow cytometry after 4-day co-culture with SKBR3 (E:T 4:1) quantified memory/activation/exhaustion states. Cytotoxicity: Live-cell imaging against GFP+ SKBR3 (2D) and MCF-7 spheroids (3D) at multiple E:T ratios quantified tumor fluorescence decline over 72 h and computed AUCs. Cytokines: 8-plex Th1/Th2 panel (GM-CSF, IFNγ, TNFα, IL-12p70, IL-4, IL-5, IL-10, IL-13) measured after 4-day co-culture (E:T 4:1). Statistical comparisons vs 28z by one-way ANOVA with Dunnett’s test.
- Library construction and expression: A 180-variant CAR signaling domain library was built; long-read sequencing confirmed 179/180 combinations with balanced representation. CARs were genomically integrated into the TRAC locus of primary human T cells, yielding monoclonal CAR expression and TCR knockout.
- scRNA-seq screen: 19,321 stimulated CAR T cells (3 donors) were profiled; 55% were assigned a single CAR variant (4% with >1 variant discarded), resulting in 10,692 annotated transcriptomes covering 156 unique variants (~2.5×10^5 reads/cell). Unsupervised clustering identified 13 T cell clusters (CD4 and CD8 subsets spanning memory, proliferative, effector, cytotoxic, terminal effector, and metabolic states). Five CAR-induced clusters (CICs) were enriched in activated CAR cells and depleted in controls.
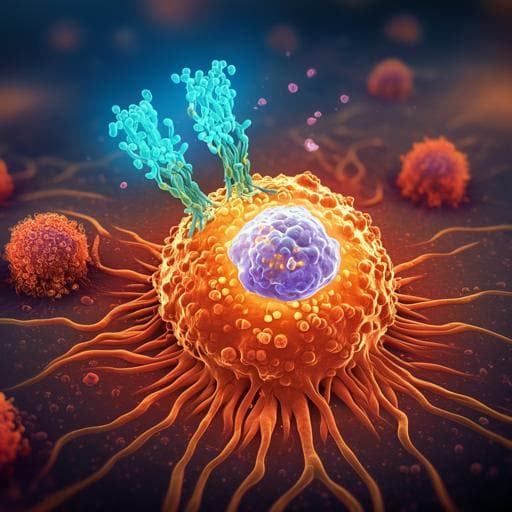
- Variant enrichment and transcriptional signatures: Many variants distributed across multiple clusters; several enriched strongly in CICs. Examples: CD30–CD79B and CD4–K1 enriched in CD8 terminal effector; CD28–FCGR2A and FCRL6–CD3G enriched in CD8 cytotoxic; 4-1BB–CD79A enriched in CD4 effector. Some (e.g., TIM1–CD79B, CD357–CD79B, CD30–CD3D) showed minimal CIC enrichment, indicating reduced potency. Pseudo-bulk PCA separated 28z/BBz from TCR− and spread variants across phenotypic space. Variants FCRL6–CD3G and CD28–FCGR2A had CD8+ phenotypes similar to 28z but reduced IFNG/CCL3/CCL4/CSF2. CD223–CD79A and FCRL6–FCGR2A expressed higher memory markers (TCF7, CD27) while maintaining effector genes, suggesting hybrid phenotypes. Gene set scoring across 18 signatures differentiated proliferation, cytotoxicity, exhaustion, memory, and tumor infiltration relative to 28z.
- Mapping to TILs: Integration with NSCLC TILs identified clusters C8 and C12 enriched in CAR CICs and TILs; both overexpressed CXCL13 and activation/tissue retention markers associated with ICB-responsive Texp/Tex states. Several CARs, including 28z, were enriched in C8/C12; some variants (e.g., 4-1BB–FCGR2A, CD244–K1, CD28–FCGR2A) showed even higher enrichment than 28z, with distinct C8:C12 ratios (e.g., CD150–CD79B, CD30–CD79B).
- Functional validation (variants A–J): Flow cytometry showed CD8+ differentiation differences; CARs E, I, J skewed to effector memory/terminal states like 28z; BBz and CARs A, G, H had larger central memory; CAR F expanded TSCM (akin to TCR−). Activation markers were generally high across CARs; all CARs increased exhaustion marker co-expression vs TCR−, with minimal differences across variants at 4 days.
- Cytotoxicity: In SKBR3 2D assays (E:T 1:1), only 28z, BBz, and CARs A–D controlled growth; at 3:1 and 8:1, all CARs controlled/eliminated tumor with distinct dynamics: A and D fastest; then B, C, 28z, BBz; E and F slightly delayed; G–I slower; J slowest. In MCF-7 spheroids, faster overall kinetics but similar rank order; CAR A most potent, followed by B, C, 28z, BBz, D, E; J consistently slowest.
- Cytokines: 28z secreted the highest pro-inflammatory cytokines (GM-CSF, IFNγ, TNFα) compared to BBz and most variants. Among A–D (fast killers), B and D resembled BBz (intermediate secretion), while A and C were even lower than BBz. E, F, G, I showed intermediate patterns with high IL-12 and IL-10; G had significantly high IL-13. H and J had lowest cytokines, resembling unstimulated controls.
- Design insights: Variants featuring Fc/Fc-like receptor domains (e.g., FCGR2A, FCER1G) and CD79B were prominent among high-performing CARs; domain synergies (e.g., TNFR family CD30, SLAM family CD150) with CD79B or CD3ζ may enhance responses. Not all constructs with CD28/4-1BB performed well when combined with specific B domains, underscoring combinatorial context effects.
The study demonstrates that combinatorial shuffling of intracellular signaling domains, coupled with pooled single-cell transcriptomic deconvolution, can rapidly explore CAR design space and uncover functional variants that differ substantially from standard 28z/BBz CARs. The scRNA-seq screen resolved multi-dimensional activation phenotypes and identified CAR-induced clusters associated with effector function. Mapping to ICB-responsive TIL states (C8/C12 with CXCL13 expression) provided a clinically relevant reference, guiding selection of variants enriched for tumor-reactive phenotypes. Functionally, several variants (A–D) matched or exceeded benchmark cytotoxicity while exhibiting reduced secretion of pro-inflammatory cytokines linked to CRS risk, suggesting potential safety advantages. The findings also reveal domain-level principles: frequent selection of Fc receptor-like domains and CD79B suggests these motifs can potentiate activation and proliferation; distinct pairings create hybrid memory-effector states that may benefit persistence without sacrificing potency. Altogether, speedingCARs addresses the research objective by offering a scalable, translatable framework to tailor CAR signaling for specific therapeutic goals, potentially aiding the development of safer, more effective CAR T products for solid tumors.
This work introduces speedingCARs, a modular domain-shuffling and pooled single-cell sequencing pipeline that expands the intracellular signaling repertoire of CARs. From a 180-variant library integrated into primary T cells, the study identified diverse transcriptional states, highlighted CAR-induced activation clusters, and mapped these to clinically relevant TIL phenotypes. Selected variants achieved potent tumor killing with distinct differentiation profiles and, in some cases, reduced pro-inflammatory cytokine secretion compared with benchmarks. The approach provides a path toward rationally selecting CAR architectures matched to clinical contexts, with potential extensions to other diseases and immune cell types. Future work should include in vivo validation, exploration of additional domain pools and antigen specificities, longer-term persistence/exhaustion studies, and systematic mapping to broader clinical single-cell atlases to refine indication-specific CAR designs.
- Translational gap: In vitro cytotoxicity and cytokine profiles may not predict clinical efficacy; no in vivo or clinical validation presented.
- Short stimulation window: 36 h for scRNA-seq and 4 days for flow/cytokines limit assessment of long-term exhaustion and persistence; authors note longer stimulation is needed to evaluate exhaustion differences.
- Expression variability: Despite TRAC targeting, CAR surface expression levels differed across variants, potentially confounding functional comparisons.
- Library coverage and assignment: Only 55–59% of cells were assigned a single CAR identity; 156/180 variants were represented in annotated data; clonal expansion evidenced some over-representation despite subsampling controls.
- Single antigen and context: All CARs shared HER2 specificity and were tested against specific lines (SKBR3, MCF-7); results may not generalize to other antigens/tumor microenvironments.
- TME modeling: In vitro co-cultures and spheroids cannot fully recapitulate complex solid tumor microenvironments.
- Potential sequence-context effects: Some domain combinations with otherwise favorable motifs performed poorly, indicating complex context dependence requiring further mechanistic study.
Related Publications
Explore these studies to deepen your understanding of the subject.