Medicine and Health
Self-promoted electroactive biomimetic mineralized scaffolds for bacteria-infected bone regeneration
Z. Li, D. He, et al.
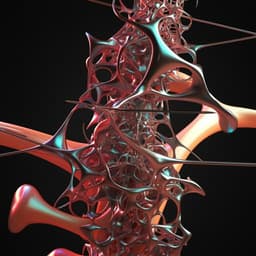
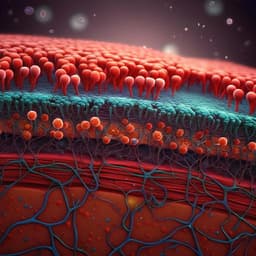
Infected bone defects pose a serious challenge in orthopedics due to high failure rates and the hindrance of regeneration by bacterial infection. In the oral cavity, open bone defects are susceptible to colonization by opportunistic pathogens; biofilm formation leads to chronic inflammation, osteoinflammatory hyperplasia, avascular necrosis, and impaired healing. Conventional management combines bone grafting with antibiotics, but drug-resistant infections and disruption of the microbiome can compromise both anti-infective efficacy and the osteoinductivity of grafts, necessitating new strategies balancing antibacterial and osteoinductive functions. Native bone exhibits piezoelectricity: endogenous weak electrical signals arise from collagen fibril polarization under shear, influencing stem cell differentiation, osteoblast behavior, and inhibiting bacterial activity by modulating voltage-gated Ca2+ channels, ATP metabolism, cytoskeletal dynamics, and membrane-associated functions. Therefore, engineered bone scaffolds should mimic not only chemical composition and micro/nanotopography but also the bioelectrical microenvironment to enhance inductive properties. In light of these considerations, the authors designed a self-promoted electroactive mineralized scaffold (sp-EMS) by biomimetic coassembly of mineralized collagen with ultrathin silver nanowires to recreate a bone-like interface capable of generating weak currents, promoting osteogenesis and angiogenesis, and inhibiting bacterial adhesion and activity without external power sources.
Materials and scaffold fabrication: Ultrathin silver nanowires (Ag uNWs) were synthesized via thermal decomposition/reduction of AgNO3 in ethylene glycol with PVP, NaBr, and benzoin; product dimensions were ~19.2 ± 4.0 nm diameter and tens of micrometers length, with Young’s modulus 0.22–0.59 GPa. Biomimetic mineralized collagen scaffolds (MS) were fabricated by self-assembly of type I tropocollagen in potassium buffer, followed by crosslinking and intrafibrillar mineralization with CaCl2, K2HPO4, and polyaspartic acid. For sp-EMS, Ag uNWs were mixed with collagen (v/v 1:19) prior to fibrillogenesis and mineralization, yielding intrafibrillar coassembly. 3D porous scaffolds were produced by casting, freezing, and lyophilization, achieving porosity 91.09 ± 1.28% and interconnected pores 117.12 ± 25.87 µm.
Characterization: TEM/HAADF-STEM/EDS confirmed D-periodic (~63.9 ± 3.3 nm) mineralized collagen with intrafibrillar Ag uNWs. ICP-OES quantified Ag mass content (~4.81–4.96%). XRD showed hydroxyapatite and metallic Ag phases. TGA differentiated Ag content via residual mass. XPS confirmed metallic Ag (Ag 3d3/2 at 374.6 eV; Ag 3d5/2 at 366.8 eV). AFM measured fibril topography and Young’s modulus (sp-EMS 9.01–13.99 GPa; similar to MS).
Electrochemical behavior: In PBS using ITO-supported films, Tafel analysis showed corrosion potential of sp-EMS at −0.03 V vs RHE vs 0.35 V for Ag uNWs, indicating accelerated corrosion due to Ag+ coordination with collagen carboxyls. Chronoamperometry showed stable microcurrent generation by sp-EMS (~−4.0 µA in PBS), whereas MS was inert. Passivated variants (Ag@AgCl and Ag@Ag2S in mineralized collagen, MS/AgCl and MS/Ag2S) were synthesized to suppress electrochemical activity; CV showed near-absent currents.
In vitro cell studies: Human bone marrow mesenchymal stem cells (BMSCs, passages 3–5) were cultured on blank (tissue culture plastic), MS, or sp-EMS. Viability and proliferation were assessed via live/dead and CCK-8. Intracellular Ca2+ influx was measured using Fluo-3 AM. Gene expression (qRT-PCR) assessed CACNA2D1, P2X7, BMP2, OCN (GAPDH housekeeping; validated with PPIA and YWHAZ). Protein analyses included Western blotting for BMP2, p-Smad1/5/9, total Smad5, F-actin, and actin; F-actin/G-actin ratios were determined by differential ultracentrifugation. Direct electrical stimulation controls used a 4 µA DC applied to culture media for 48 h.
Antibacterial assays: Staphylococcus aureus (CGMCC1.6722) was incubated with scaffold-coated wells. Antimicrobial efficacy was evaluated by CFU counting, live/dead staining, SEM/TEM of bacterial morphology, ROS generation (DCFH-DA fluorescence), and Ag+ release profiles (ICP-OES) over 14 days. Passivated scaffolds (MS/AgCl, MS/Ag2S) served to isolate the role of electrical activity.
Inflammatory milieu osteogenesis: BMSCs were cultured in osteogenic medium with S. aureus-derived LTA (10 µg/mL) to assess inflammatory markers (TNF-α, iNOS) and osteogenic genes (BMP2, OCN).
In vivo models and assessments:
- Rat noninfected calvarial critical-sized defects (5 mm): groups were blank, MS, sp-EMS (n=5/group). Outcomes at 8 and 12 weeks via µCT (bone volume, new bone area/total area) and histology (HE, Masson), plus safety (organ histology; silver biodistribution/excretion by ICP-OES). In situ microcurrent measurements were taken on days 1, 3, 7, 14, 21. Immunofluorescence for CACNA2D1 at 2 weeks; immunohistochemistry for BMP2, OCN, VEGFR-1, CD31 at 8 weeks.
- Rat infected calvarial defects: 5 mm defects inoculated with 100 µL S. aureus (1×10^6 CFU/mL); groups blank, MS, sp-EMS (n=5/group). Outcomes at 12 weeks (µCT, histology) and 2 weeks (immunofluorescence for TNF-α, iNOS, CD68, CD163 to assess inflammation and macrophage polarization).
- Rabbit open alveolar defects: bilateral mandibular first premolar extractions with sockets left open to oral cavity; groups blank, MS, sp-EMS (n=3/group). Outcomes at 8 weeks: µCT (BV/TV, BMD, trabecular thickness), histology.
- Beagle dog vertical mandibular defects: post-extraction atrophy followed by creation of 10×10×8 mm^3 defects; groups blank, MS, sp-EMS, Bio-Oss collagen (n=3/group). Outcomes at 12 weeks: µCT (BV/TV, vertical bone height, BMD), histology.
Statistics: Experiments repeated ≥3 times; data as mean ± SD. Student’s t-test or one-way ANOVA with Tukey’s post hoc; significance at P<0.05. Animal sample sizes justified by prior power analyses (rats) or resource equation (rabbits/dogs).
- Physicochemical/electroactive properties: sp-EMS achieved intrafibrillar coassembly of Ag uNWs within mineralized collagen fibrils (D-period ~63.9 nm). Ag content
4.8–5.0% by ICP-OES/TGA. Corrosion potential: sp-EMS −0.03 V vs RHE vs Ag uNWs 0.35 V, indicating facilitated electrochemical corrosion via collagen–Ag+ coordination. sp-EMS generated stable microcurrents (−4.0 µA in PBS); MS inert. Passivation (AgCl or Ag2S) abolished electrical signals. - In vitro biocompatibility and osteoinduction: BMSC viability ~98.95 ± 1.02% on sp-EMS (comparable to MS and blank) and proliferation increased through day 7. sp-EMS enhanced Ca2+ influx (Fluo-3), upregulated CACNA2D1 and P2X7 mRNA at days 7 and 14 (P<0.001 vs MS/blank), increased F-actin and F/G-actin ratio (P<0.001), and elevated osteogenic markers BMP2 and OCN (qPCR) and BMP2 and p-Smad1/5/9 proteins (WB). Passivation (MS/AgCl, MS/Ag2S) reduced Ca2+ influx, CACNA2D1/P2X7, F/G-actin, BMP2/OCN, and p-Smad1/5/9 (P<0.001), confirming dependence on electrical stimulation. Direct DC stimulation (4 µA, 48 h) recapitulated sp-EMS effects on Ca2+, CACNA2D1, P2X7, F/G-actin, BMP2/OCN, and p-Smad1/5/9.
- Antibacterial activity: sp-EMS strongly inhibited S. aureus growth (reduced CFUs), killed bacteria (live/dead: 74.50 ± 4.96% dead vs MS 3.79% dead; blank 1.69% dead), prevented adhesion (SEM) and disrupted membranes (TEM). Passivation eliminated antibacterial effect (P<0.001 vs sp-EMS). Mechanistically, sp-EMS released Ag+ continuously over 14 days and increased ROS (DCF-DA fluorescence 2.23× vs MS and 3.29× vs blank at 6 h; P<0.001), indicating synergistic electrochemical antibacterial action. Under LTA-induced inflammatory conditions, sp-EMS downregulated TNF-α and iNOS and upregulated BMP2 and OCN in BMSCs at days 7 and 14.
- Rat noninfected calvarial defects: At 8 weeks, new bone area/total area: sp-EMS 77.45 ± 2.88% vs MS 31.55 ± 8.22% vs blank 6.17 ± 2.53% (P<0.001); bone volume: sp-EMS 60.80 ± 2.26 mm³ vs MS 24.77 ± 6.45 mm³ vs blank 4.84 ± 1.99 mm³. At 12 weeks, near-complete healing: sp-EMS 96.93 ± 6.22% vs MS 67.74 ± 5.77% vs blank 12.24 ± 4.14% (P<0.001); bone volume: 76.12 ± 4.89 mm³ vs 54.48 ± 5.63 mm³ vs 9.85 ± 3.04 mm³. Histology showed dense, vascularized bone in sp-EMS group with near-complete degradation of scaffold and no Ag residues detectable; organ histology showed no liver/kidney toxicity; silver cleared via urine/feces; negligible residual silver at 12 weeks. In situ microcurrents on sp-EMS: −4.5 µA (24 h), −4.0 µA (day 3), −3.0 µA (day 7), −2.0 µA (day 14), −0.02 µA (day 21). Increased CACNA2D1+ cells at 2 weeks: 18.02 ± 4.32% (sp-EMS) vs 2.28 ± 0.87% (MS) vs 0.00 ± 0.01% (blank; P<0.001). Elevated BMP2, OCN, VEGFR-1, and CD31 in sp-EMS at 8 weeks.
- Rat infected calvarial defects: At 12 weeks, sp-EMS achieved near-complete repair by µCT/histology. New bone area/total area: sp-EMS 89.16 ± 11.16% vs MS 32.64 ± 5.29% vs blank 6.06 ± 1.68% (P<0.001). New bone volume: sp-EMS 70.01 ± 8.74 mm³ vs MS 25.63 ± 4.15 mm³ vs blank 4.77 ± 1.32 mm³ (P<0.001). At 2 weeks, reduced inflammation: TNF-α+ cells 3.87 ± 3.02% (sp-EMS) vs MS 48.22 ± 12.21% vs blank 58.69 ± 4.05% (P<0.001); similar trend for iNOS. Macrophage polarization favored M2: CD68+CD163+ M2 64.81 ± 6.12% (sp-EMS) vs 10.74 ± 0.53% (MS) vs 6.64 ± 0.49% (blank; P<0.001); M1 (CD68+iNOS+) reduced to 5.51 ± 2.26% vs 41.16 ± 8.60% vs 53.49 ± 2.94% (P<0.001).
- Rabbit open alveolar defects (8 weeks): sp-EMS produced nearly complete regeneration with BV/TV ~98.38%, BMD 0.49 ± 0.06 g/cm³ (vs natural trabecular bone 0.54 ± 0.02), trabecular thickness 0.27 ± 0.02 mm. MS: BV/TV ~76.90%, BMD 0.28 ± 0.01 g/cm³, Tb.Th 0.19 ± 0.01 mm. Blank: BV/TV ~66.65%, BMD 0.16 ± 0.01 g/cm³, Tb.Th 0.11 ± 0.01 mm. Histology showed extensive vascularized bone and organized collagen fibers in sp-EMS.
- Beagle dog vertical defects (12 weeks): sp-EMS achieved BV/TV 85.20 ± 4.23%, vertical bone height 6.42 ± 0.16 mm, BMD 0.35 ± 0.04 g/cm³, outperforming MS (BV/TV 62.55 ± 3.76%, height 5.01 ± 0.63 mm, BMD 0.26 ± 0.03 g/cm³), Bio-Oss (BV/TV 54.80 ± 2.17%, height 4.70 ± 0.34 mm, BMD 0.19 ± 0.01 g/cm³), and blank (BV/TV 31.69 ± 4.36%, height 2.79 ± 0.23 mm, BMD 0.04 ± 0.02 g/cm³). Histology confirmed robust vascularized bone with near-complete vertical defect repair in sp-EMS.
The study addresses the challenge of simultaneously achieving osteogenesis and antibacterial activity in infected bone defects by recreating bone’s bioelectrical microenvironment. The sp-EMS integrates a bone-like mineralized collagen interface with embedded ultrathin Ag nanowires that self-generate mild, sustained microcurrents via electrochemical corrosion without external power. This endogenous-like stimulation activates VGCC-mediated Ca2+ influx, enhances ATP production, drives actin cytoskeletal remodeling, and upregulates BMP2/Smad signaling, promoting osteogenic differentiation and angiogenesis. Concurrently, electrochemical products (Ag+) and ROS inhibit bacterial adhesion and viability, alleviating inflammation and favoring M2 macrophage polarization in vivo. Across small and large animal models—including complex oral microenvironments—sp-EMS enabled complete or near-complete in situ bone regeneration with appropriate biodegradation and biosafety, surpassing conventional mineralized scaffolds and a clinical control (Bio-Oss). These results demonstrate that circuit-free, self-powered electroactive scaffolds can overcome limitations of piezoelectric materials (heterogeneous interfaces, dependence on external excitation, potential cytotoxicity) and device-based stimulation (implant complexity, power delivery constraints), offering a translational platform for complex defect repair.
This work introduces a self-promoted electroactive mineralized scaffold that combines a biomimetic bone-like interface with embedded ultrathin silver nanowires to provide continuous, mild electrical stimulation in situ. The sp-EMS orchestrates osteogenesis and angiogenesis via Ca2+ influx and BMP2/Smad signaling while concurrently exerting potent antibacterial effects through Ag+ release and ROS generation. The scaffold degrades in concert with new bone formation and exhibits favorable biosafety, achieving complete or near-complete regeneration in infected rat calvarial defects, rabbit open alveolar defects, and beagle dog vertical mandibular defects. Future research could explore performance against diverse and antibiotic-resistant pathogens, long-term outcomes and functional integration under load-bearing conditions, optimization of electrical output and degradation kinetics for various defect types, and scalable manufacturing and sterilization processes for clinical translation.
- Pathogen scope: In vitro antibacterial testing focused on Staphylococcus aureus; broader evaluation against polymicrobial and antibiotic-resistant species is warranted.
- Sample size and power: Large-animal studies (rabbits, dogs) used n=3 per group via a resource equation approach; formal power analyses and larger cohorts would strengthen generalizability.
- Comparative therapies: Direct comparisons with antibiotic-loaded grafts or other electroactive/piezoelectric materials were limited, constraining benchmarking.
- Long-term safety: Although silver clearance and organ histology were favorable up to 12 weeks, extended biodistribution, systemic exposure, and immunological assessments over longer periods remain to be established.
- Mechanistic depth: While BMP2/Smad and cytoskeletal remodeling were implicated, comprehensive mapping of downstream pathways and cell-type-specific responses in vivo could further elucidate mechanisms.
Related Publications
Explore these studies to deepen your understanding of the subject.