Medicine and Health
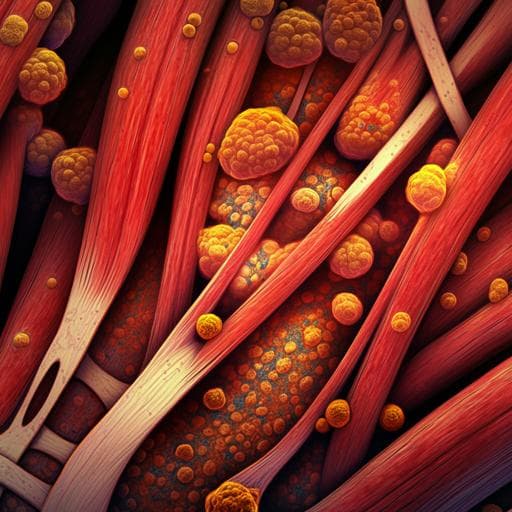
Myosteatosis and sarcopenia are linked to autonomous cortisol secretion in patients with aldosterone-producing adenomas
B. Lee, Y. Chang, et al.
This research explores the impact of autonomous cortisol secretion on muscle health in patients with adrenal aldosterone-producing adenomas. Conducted by a team of experts including Bo-Ching Lee and colleagues, the study reveals significant changes in intermuscular adipose tissue and skeletal muscle area following adrenalectomy, highlighting the links between ACS, myosteatosis, and sarcopenia.
Related Publications
Explore these studies to deepen your understanding of the subject.