Medicine and Health
Mucosal TLR2-activating protein-based vaccination induces potent pulmonary immunity and protection against SARS-CoV-2 in mice
A. S. Ashhurst, M. D. Johansen, et al.
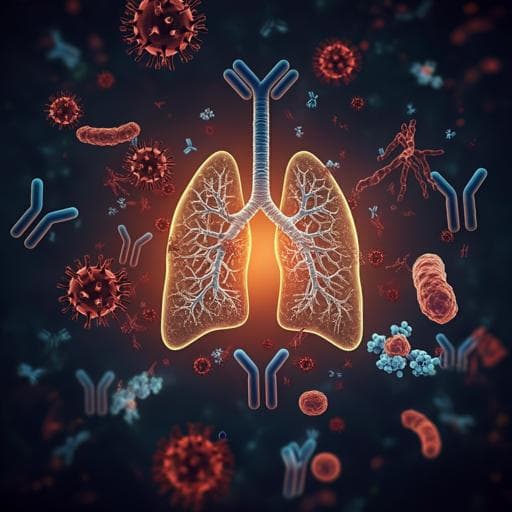
The study addresses the need to enhance protection against SARS-CoV-2 infection and transmission, which remains suboptimal with current intramuscular vaccines that primarily elicit systemic IgG and T-cell responses but limited mucosal immunity. Given waning immunity and immune-evasive variants, the authors hypothesize that mucosal vaccination with a protein subunit vaccine adjuvanted with a TLR2 agonist (Pam₂Cys) can induce robust local (respiratory) immunity, including secretory IgA and tissue-resident T cells, thereby improving barrier protection in the upper and lower respiratory tract. The work evaluates immunogenicity, the role of TLR2 on epithelial versus hematopoietic compartments in vaccine responses, and protective efficacy against SARS-CoV-2 in mice.
Prior work shows intranasal vaccination can elicit mucosal IgA and resident memory B/T cells that reduce infection and shedding in respiratory pathogens, including SARS-CoV-2, often using live-attenuated or viral vectors, which face safety and boosting limitations. Protein vaccines can be safer and broadly applicable but require effective mucosal adjuvants. TLR2 is expressed by respiratory epithelia and immune cells and is important in host defense. Pam₂Cys, a TLR2 ligand, has previously acted as an effective mucosal adjuvant with peptide/protein vaccines against Mycobacterium tuberculosis and provided short-term non-specific antiviral protection when delivered intranasally in other models. These data motivate testing a Pam₂Cys-adjuvanted Spike protein for mucosal vaccination against SARS-CoV-2.
Vaccine: Recombinant trimeric SARS-CoV-2 Spike HexaPro protein (Addgene #154754) produced in Expi293F cells and purified by IMAC and gel filtration was admixed with Pam₂Cys-SK4-triethylene glycolate (TLR2 agonist). Dose per vaccination: 6 µg Spike + 7.7 µg Pam₂Cys in PBS. Animals and immunization: Female C57BL/6 mice and K18-hACE2 mice were immunized either subcutaneously (s.c., base of tail) or intranasally (i.n.) under anesthesia. Regimens included single i.n. dose for innate response profiling and three homologous immunizations 2 weeks apart (or 2.5 weeks in sustained protection study). Immune responses assessed 1 week and 8 weeks post-final boost. For mechanistic studies, TLR2 bone marrow chimeric BALB/c mice were generated by lethal irradiation and reconstitution with WT or Tlr2−/− bone marrow to create combinations with TLR2 expression on immune, non-immune, both, or neither compartments; mice rested 12 weeks before vaccination. Immunogenicity assays: Serum and bronchoalveolar lavage fluid (BALF) collected; Spike-specific IgG, IgG1, IgG2c, IgA (and IgE) quantified by ELISA with titers interpolated against mean +3 SD of controls. Neutralization: pseudovirus assay using SARS-CoV-2 Spike-pseudotyped lentivirus infecting HEK293-ACE2 cells; and live-virus neutralization in VeroE6 or HEK-ACE2-TMPRSS2 cells versus ancestral, Beta, Delta, and Omicron BA.5 variants; EC50 defined as dilution giving ≥50% inhibition. Cellular immunity: Ex vivo recall of leukocytes from lungs, spleen, and mediastinal lymph nodes (MLN); intracellular cytokine staining (ICS) for IFNγ, IL-2, IL-4, IL-17A, TNF after stimulation with whole Spike or CD8 epitope Spike338–346; flow cytometry to enumerate cytokine-producing CD4+/CD8+ T cells and TRM-like cells (CD4+ or CD8+ CD69+CD44+CD62L−; CD8 TRM also CD103+). Computational clustering of CD45+ lung cells with FlowSOM and FIt-SNE using Spectre R package; manual gating for myeloid and lymphoid subsets. BALF cytokines measured by Legendplex. Challenge studies: K18-hACE2 mice vaccinated s.c. or i.n. with Pam₂Cys alone or Pam₂Cys+Spike, then challenged intranasally with SARS-CoV-2 (VIC01/2020). Early challenge at 3 weeks post-final boost; sustained protection assessed at 6 weeks post-final boost. Outcomes: body weight, clinical scores, BALF leukocyte differentials, lung histology, and lung viral titers by plaque assay (PFU). Statistical analyses: Mann–Whitney, Welch’s t-test, Kruskal–Wallis with Dunn’s, two-way ANOVA with Tukey’s; significance at p≤0.05.
- Both s.c. and i.n. Pam₂Cys+Spike vaccinations induced high anti-Spike IgG (IgG1, IgG2c) in serum and BALF; mucosal (i.n.) route produced significantly higher BALF IgG and uniquely induced robust anti-Spike IgA in serum and BALF (titers up to ~10^6–10^7 in BALF), with no significant IgE.
- Neutralizing antibodies (nAb) were strong in serum for both routes but significantly higher with i.n.; only i.n. vaccination yielded substantial nAb in airways (BALF). High nAb titers against ancestral virus were maintained at 8 weeks; serum nAb to Delta retained (not to Omicron BA.5), with i.n. showing advantages. In K18-hACE2, i.n. vaccination generated mean nAb EC50 >10^3 against Beta and Delta.
- Cellular immunity: i.n. vaccination elicited prominent lung Spike-specific CD4+ T cells producing IL-17A at 1 week post-boost and diverse CD4+ responses in spleen (IL-2, IL-17, TNF). At 8 weeks, lung Spike-specific CD4+ (IL-2, IL-17, TNF) and CD8+ (IFNγ, TNF) responses persisted in i.n.-vaccinated mice, with marked lung TRM-like populations, especially CD4+ TRM (~25-fold more frequent than CD8+ TRM).
- TLR2 compartmental roles: After single i.n. dose, TLR2 expression on either epithelial (non-immune) or hematopoietic compartments was sufficient for early neutrophil recruitment and increased lung leukocytes at 24 h; epithelial TLR2 favored recruitment of APCs (DCs, alveolar macrophages, monocyte subsets). Hematopoietic TLR2 drove early airway cytokines (TNF, IL-6).
- Adaptive responses required hematopoietic TLR2: Following triple i.n. vaccination, groups with TLR2 on immune cells showed significantly greater lung T-cell numbers (notably CD4+), higher Spike-specific IgG/IgA titers, higher nAb in serum and BALF, increased MLN Bcl6+ CD4+ Tfh, and elevated lung Spike-specific CD4+ IL-17A and TNF+ cells. Optimal responses occurred when TLR2 was present on both compartments.
- Protection: Both s.c. and i.n. Pam₂Cys+Spike conferred complete protection in K18-hACE2 mice against clinical disease and induced sterilizing lung immunity (no detectable PFU at day 7). Notably, Pam₂Cys i.n. alone conferred short-term non-specific protection (40% no weight loss; 60% with no detectable lung virus at day 7), which was not sustained at 6 weeks. Vaccinated mice showed reduced BALF inflammatory cell influx and reduced histological lung inflammation.
- Variant breadth: While Delta neutralization was preserved (especially with i.n.), neutralization against Omicron BA.5 was largely lost, indicating immune evasion for this variant.
Findings demonstrate that a protein subunit vaccine comprising Spike with a TLR2 agonist (Pam₂Cys) can, when delivered mucosally, generate robust local mucosal immunity (secretory IgA, elevated airway nAb, lung TRM and Th17 responses) alongside systemic antibody responses, thereby addressing the gap in upper and lower respiratory tract protection left by parenteral vaccines. Mechanistic studies reveal that TLR2 signaling in both epithelial and immune compartments contributes to innate recruitment, whereas hematopoietic TLR2 is crucial for optimal adaptive immunity, aligning with the role of APCs and Tfh/Th17 in mucosal vaccine efficacy. The sterilizing protection in lungs and abrogation of disease in the stringent K18-hACE2 model correlate with strong nAb responses and local immunity, supporting mucosal vaccination to reduce infection and potential transmission. The transient non-specific protection from intranasal Pam₂Cys alone underscores innate priming in the airway but also the necessity of antigen-specific immunity for durable protection. Limited neutralization of Omicron BA.5 highlights variant-driven immune escape and the need to update antigenic content or include conserved epitopes.
A mucosal, TLR2-activating, protein-based Spike vaccine induces potent humoral and cellular immunity in the respiratory tract and provides sterilizing lung protection against SARS-CoV-2 in mice. TLR2 on hematopoietic cells is required for optimal adaptive responses, while epithelial and immune TLR2 both support early innate recruitment. Intranasal delivery uniquely elicits IgA, airway nAb, and lung TRM/Th17 responses, offering advantages for blocking infection and spread. Future directions include optimizing antigen design for variant breadth (e.g., conserved Spike epitopes), incorporating additional antigens (e.g., nucleocapsid) to broaden T-cell immunity, assessing durability and upper airway protection, evaluating impact on transmission in relevant models, and exploring heterologous prime–mucosal boost strategies for populations previously vaccinated intramuscularly.
- Conducted in mouse models (including K18-hACE2), which may not fully recapitulate human immunity or clinical outcomes.
- Limited breadth against immune-evasive variants (e.g., Omicron BA.5 showed loss of neutralization), indicating need for updated antigens.
- Durability of mucosal and systemic protection beyond the tested intervals requires further study, particularly in the upper respiratory tract (nasal passages, trachea).
- Transmission reduction was not directly assessed; requires studies in models suited for transmission (hamster, ferret).
- Intranasal delivery parameters (dose/volume, URT vs LRT targeting) and safety/tolerability in humans need evaluation.
- Non-specific protection from Pam₂Cys alone was transient and absent by 6 weeks, underscoring the need for antigen-specific immunity for sustained protection.
Related Publications
Explore these studies to deepen your understanding of the subject.