Medicine and Health
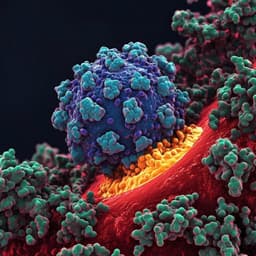
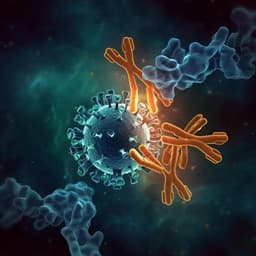
Molecular interaction and inhibition of SARS-CoV-2 binding to the ACE2 receptor
J. Yang, S. J. L. Petitjean, et al.
This study reveals the intricate binding mechanism of SARS-CoV-2 spike glycoprotein to the ACE2 receptor using atomic force microscopy. The researchers identify the receptor-binding domain as the key interaction site and explore potential peptide inhibitors for therapeutic applications, conducted by Jinsung Yang, Simon J. L. Petitjean, Melanie Koehler, Qingrong Zhang, Andra C. Dumitru, Wenzhang Chen, Sylvie Declercq, Stéphane P. Vincent, Patrice Soumillion, and David Alsteens.
Related Publications
Explore these studies to deepen your understanding of the subject.