Medicine and Health
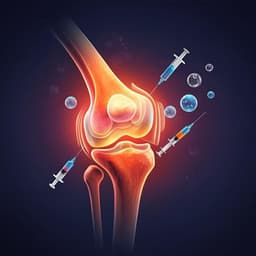
Mesenchymal stem cell-derived exosomes as a promising cell-free therapy for knee osteoarthritis
D. Luo, H. Zhu, et al.
Osteoarthritis (OA) is a debilitating disease with substantial socioeconomic implications. Current treatments primarily alleviate symptoms rather than addressing disease progression. This innovative study, conducted by Danni Luo and colleagues, delves into the potential of mesenchymal stem cell-derived exosomes in OA treatment, revealing mechanisms, strategies, and future challenges.
Related Publications
Explore these studies to deepen your understanding of the subject.