Medicine and Health
Lactobacillus fermentum LM1016 Ameliorates Diet-Induced Obesity by Modulating Bile Acid Signaling and Adipose Tissue Inflammation
Y. Y, K. G, et al.
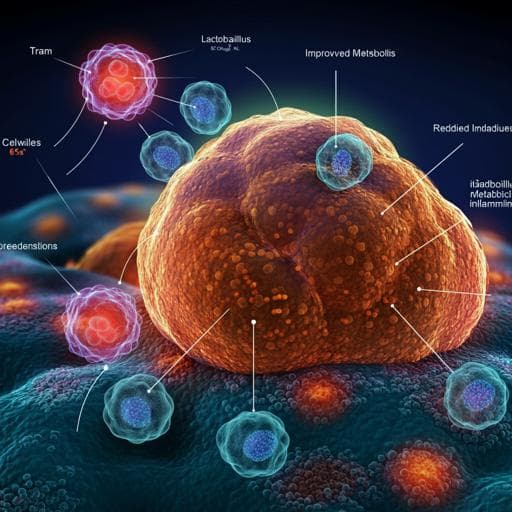
The study addresses how specific Lactobacillus strains, particularly Lactobacillus fermentum LM1016, protect against high-fat diet (HFD)-induced obesity and related metabolic dysfunction. While prior work has shown various Lactobacillus spp. can improve metabolic biomarkers (glucose, insulin, triglycerides), the underlying mechanisms remain unclear. This work evaluates the anti-obesity efficacy of L. fermentum LM1016 and investigates mechanisms spanning bile acid signaling, adipose tissue thermogenesis and inflammation, hepatic metabolism, and bacterially derived metabolites.
Background literature cited links gut microbiota to obesity, inflammation, and metabolic regulation. Prior studies report certain Lactobacillus strains reduce adiposity and improve metabolic markers in animals and humans. Oxidative stress and redox balance are implicated in metabolic syndromes. Bile acids can drive energy expenditure via TGR5-mediated potentiation of thyroid hormone signaling in brown adipose tissue (BAT). Intestinal FXR–FGF15 signaling suppresses hepatic bile acid synthesis. Previous reports also show that specific fatty acids (e.g., vaccenic acid, conjugated linoleic acid) exert hypolipidemic and anti-obesity effects. However, genetic and metabolomic mechanisms for Lactobacillus-mediated anti-obesity effects were not fully elucidated.
In vivo mouse model: Male C57BL/6N mice (6 weeks old) acclimated 1 week and fed either a normal diet (ND), high-fat diet (HFD; 60% kcal fat, D12492), or HFD plus probiotics for 8 weeks. Daily oral gavage of 1×10^9 CFU per mouse of Lactobacillus strains in PBS (L. fermentum LM1016; L. acidophilus Rosell418 and La14; L. salivarius Lrs-33; L. rhamnosus HOWARU; L. paracasei LPC37; L. helveticus LH166). Body weight weekly; terminal collection of blood and tissues (liver, gonadal WAT, inguinal WAT, BAT). Colonization: Single 1×10^9 CFU oral dose; fecal collection at 4, 8, 12, 24 h; DNA extraction (FastDNA SPIN Kit); qPCR with L. fermentum-specific primers normalized to 16S rRNA. Histology: Liver, BAT, gWAT fixed, paraffin-embedded, sectioned (4 μm), H&E staining. Liver triglycerides: NP-40 extraction; colorimetric assay (Abcam). Gene expression: TRIzol RNA extraction; cDNA synthesis (PrimeScript); qPCR on Bio-Rad CFX384 with SYBR; 95°C 10 min, 35 cycles of 95°C 10 s, 60°C 15 s, 72°C 15 s; normalization to 36B4. Serum biochemistry: Insulin and leptin by ELISA (Morinaga); total cholesterol (Mindray BS-200); bile acids (Sigma enzymatic assay); CRP (R&D Quantikine). Glucose tolerance tests: 12 h fast, 2 g/kg i.p. glucose, glucose at 0–120 min. Tissue transcriptomics and GSEA: Intestinal RNA (Qiagen RNeasy); libraries (Illumina TruSeq v2); HiSeq 2500, 101-bp PE; alignment to GRCm38 (STAR); quantification (RSEM); GSEA (javaGSEA v2.1.0) using GO BP sets (15–500 genes), 1000 permutations; significant if Q<0.25. Plasma metabolomics: Protein precipitation with 80% methanol; UPLC-Q-TOF/MS (Waters Synapt G2Si), BEH C18 column; gradient 0–100% B over 10.5 min; ESI+/−; m/z 60–1400; data by Progenesis QI; IDs via exact mass/MSMS and HMDB, METLIN, MassBank, LIPID MAPS. Bacterial transcriptomics and functional annotation: L. fermentum RNA (ZymoBIOMICS); rRNA depletion (Ribo-Zero); HiSeq 2500; mapping to NC010610.1 (STAR); counts (Cufflinks); functional grouping by ClueGO (kappa>0.4; E. coli BP; Bonferroni step-down). Bacterial extract preparation: L. fermentum LM1016 grown in MRS; washed; lysed (FastPrep-24 5G); supernatant filtered 0.2 μm. In vitro adipogenesis: 3T3-L1 preadipocytes cultured in DMEM; differentiation induced (IBMX, dexamethasone, insulin); from day 2, treated with 1% bacterial extract or 10 μg/mL linoleic acid; Oil Red O on day 10. Macrophage assays: RAW 264.7 cells treated with LPS (100 ng/mL) ± 1% bacterial extract for 24 h; IL-6 and TNF-α measured by ELISA; inflammatory gene expression assessed by qPCR. Statistics: Two-way ANOVA for body weight and GTT; Student’s t-test or one-way ANOVA for group comparisons; data shown as mean ± SEM; significance thresholds as reported in figures (e.g., p<0.05, p<0.01, p<0.001).
- Among seven Lactobacillus strains tested in HFD-fed mice, only L. fermentum LM1016 significantly reduced HFD-induced body weight gain compared with vehicle; other strains showed no anti-obesity effect (two-way ANOVA, p<0.001). L. fermentum transiently localized in the gut for several hours post-gavage and was undetectable by 24 h, implying need for daily dosing. - BAT thermogenesis: L. fermentum LM1016 reduced lipid droplet size in BAT and increased thermogenic and oxidative genes (Ucp1, Dio2, Acadm, Esrr, Aox) in BAT (p<0.05 to p<0.001). - Bile acid signaling: Serum bile acids increased with L. fermentum treatment (p<0.01 to p<0.001). Hepatic bile acid synthesis genes Cyp7a1 and Cyp27a1 were upregulated (p<0.05 to p<0.01). Intestinal FXR target genes Fgf15, Ibabp, and Ostβ were suppressed in ileum and colon (p<0.05 to p<0.001), consistent with disinhibition of hepatic bile acid synthesis and enhanced BAT energy expenditure. - Glucose homeostasis and metabolic markers: L. fermentum LM1016 improved glucose tolerance (two-way ANOVA, p<0.01 to p<0.001), reduced fasting insulin, leptin, and total cholesterol levels versus HFD vehicle (p<0.01 to p<0.001). - Serum metabolomics: L. fermentum altered plasma metabolites, increasing avenoleic acid, 2R-hydroxy-oleic acid, and specific phosphatidylcholines, while decreasing 20:3 cholesteryl ester (associated with adiposity/insulin sensitivity). - Liver: Reduced liver weight (p<0.05), decreased hepatic triglyceride content (p<0.01) and lipid droplet size, and downregulated hepatic genes involved in gluconeogenesis, lipogenesis, and lipid sequestration (p<0.05 to p<0.001), indicating amelioration of hepatic steatosis. - Adipose tissue mass/inflammation: Reduced iWAT and gWAT weights (p<0.05 to p<0.01) and adipocyte size. In gWAT, inflammatory markers (F4/80, Mcp1, Tgfβ, Ifnγ, Il1β, Il18) were significantly decreased (p<0.05 to p<0.001). Serum CRP was reduced, indicating lower systemic inflammation. - gWAT transcriptomics (GSEA): Oxidative phosphorylation gene sets were enriched/upregulated in L. fermentum-treated HFD mice (FDR q=0.000), while inflammatory pathways including TNFα signaling via NF-κB, inflammatory response, and allograft rejection were downregulated (FDR q=0.003–0.013). Colonic transcriptomics similarly showed reduced inflammatory signaling. - Bacterial metabolite production: Metabolomics of L. fermentum LM1016 culture supernatant identified 12 metabolites absent from MRS media, including linoleic acid, vaccenic acid, and ethyl pentadecanoate (all p<0.01 to p<0.001). - In vitro mechanisms: L. fermentum extracts reduced 3T3-L1 adipocyte differentiation and lipid accumulation and downregulated adipogenesis genes (Pparγ, Fas, adiponectin) (p<0.05 to p<0.001). Extracts attenuated LPS-induced IL-6 secretion in 3T3-L1 cells (one-way ANOVA). Linoleic acid (10 μg/mL) inhibited adipocyte differentiation and lipid accumulation and reduced Scd1 and Srebp1 expression (p<0.01 to p<0.001). In RAW 264.7 macrophages, both extracts and linoleic acid suppressed inflammatory genes (IL-1β, TNF-α, F4/80, Mcp1) and reduced secreted TNF-α protein.
The findings demonstrate that daily oral administration of L. fermentum LM1016 counters HFD-induced obesity through coordinated effects on host metabolic and inflammatory pathways. Enhanced BAT thermogenesis and energy expenditure appear linked to increased systemic bile acids and upregulation of hepatic bile acid synthesis, likely via suppression of intestinal FXR–FGF15 signaling. In adipose tissue, L. fermentum shifts transcriptional programs toward oxidative phosphorylation while dampening inflammatory pathways, aligning with improvements in systemic metabolic markers (glucose, insulin, leptin, cholesterol) and reduced CRP. The microbiome-derived metabolites, notably linoleic acid and vaccenic acid identified in L. fermentum supernatants, likely contribute to anti-adipogenic and anti-inflammatory effects, as validated in 3T3-L1 and RAW 264.7 cells. Together, these results address the initial hypothesis by establishing mechanistic links between a specific Lactobacillus strain, bile acid metabolism, adipose tissue bioenergetics, and systemic inflammation in the attenuation of diet-induced obesity.
Administration of L. fermentum LM1016 protects against HFD-induced obesity, improves glucose tolerance, and lowers insulin, leptin, and cholesterol. Mechanistically, it enhances BAT thermogenesis via increased bile acids and hepatic bile acid synthesis (with suppression of intestinal FXR–FGF15 signaling), reduces hepatic steatosis by downregulating gluconeogenic/lipogenic programs, and promotes oxidative phosphorylation while suppressing inflammation in adipose tissue. L. fermentum produces metabolites (e.g., linoleic and vaccenic acids) that inhibit adipogenesis and inflammatory signaling in vitro, suggesting a metabolite-mediated component. These findings support L. fermentum LM1016 as a potential therapeutic for metabolic disorders. Future work could include: causal validation of specific metabolites in vivo; receptor/pathway dissection (e.g., TGR5, FXR) using knockout models; dose–response and durability studies; assessment of colonization dynamics; and translation to human clinical trials to evaluate efficacy and safety.
Explicit limitations were not detailed in the provided text. Potential considerations include reliance on a single mouse strain and HFD model, transient intestinal localization suggesting continued dosing is required, limited direct causal linkage between individual metabolites and in vivo effects, lack of microbiome compositional profiling beyond L. fermentum detection, and absence of human data.
Related Publications
Explore these studies to deepen your understanding of the subject.