Medicine and Health
Fully bioresorbable hybrid opto-electronic neural implant system for simultaneous electrophysiological recording and optogenetic stimulation
M. Cho, J. Han, et al.
The paper addresses the need for neural interfaces that can both monitor and modulate brain activity with high spatial and temporal precision while avoiding long-term implantation risks and the need for secondary removal surgeries. Conventional micro-neural implant electronics (µ-NIE) fabricated from rigid inorganic materials (e.g., silicon, metals with Young's modulus >100 GPa) cause mechanical mismatch with soft brain tissue (~3 kPa), inducing tissue damage and immune responses. Advances in flexible and soft neural implants have improved biocompatibility but still require surgical extraction after use. Optogenetics enables cell-type-specific, temporally precise stimulation with reduced interference during electrophysiological recordings compared to electrical stimulation. Bioresorbable implants offer transient operation followed by complete dissolution, eliminating removal procedures; however, most prior systems are single-function and integrating multiple modalities (recording and stimulation) poses material, electrical, and mechanical challenges. The authors propose a fully bioresorbable hybrid opto-electronic device that integrates a PLGA optical waveguide with a biodegradable Mo/Si bilayer electrode array to enable simultaneous optogenetic stimulation and electrophysiological recording, optimized to minimize optical losses and photoelectric artifacts.
Prior work has developed µ-NIEs and optogenetic tools for neural interfacing, including integrated optical stimulation and recording probes. Rigid devices lead to glial scarring and neuronal loss, motivating flexible and soft implants based on nanomaterials, polymers, and thin films to improve biocompatibility and conformal contact. Bioresorbable electronics have been demonstrated for brain mapping, physical sensing (temperature, pressure, blood flow), chemical sensing (e.g., dopamine), electrical stimulation (peripheral and spinal), and optical stimulation with biodegradable optical components. Despite these advances, existing bioresorbable systems are largely single-function. Multifunctional transient systems face issues of material integration (differing mechanical/electrical properties leading to failure or cross-interference) and fabrication complexity. The present work builds upon bioresorbable Si electronics, PLGA optical waveguides, and strategies to mitigate photoelectric artifacts by adding an opaque metal layer, advancing to a monolithically integrated, transient hybrid system optimized for artifact-free opto-electrophysiology.
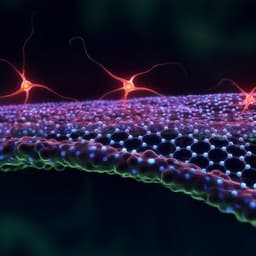
Device design and materials: The system integrates a soft, biodegradable poly(lactic-co-glycolic acid) (PLGA) waveguide (n≈1.47, ~100 µm embossed features on a 20 µm substrate) with a 6-channel electrocorticography (ECoG) electrode array. Electrodes are a Mo (300 nm)/highly P-doped Si (300 nm) bilayer nanomembrane with an outer SiO2 encapsulation layer (150 nm) for insulation and moisture barrier. The Si is n-type to reduce resistivity and low-frequency losses. The electrode recording sites are grid-shaped (line width 10 µm, typical fill factors 42–63%, area 280 × 280 µm²) to allow optical windows for stimulation. Optical coupling and waveguiding: A 460 nm laser is coupled via a step-index multimode optical fiber (core 105 µm) to the PLGA waveguide. Light propagation relies on total internal reflection (TIR) at the PLGA–cerebrospinal fluid (CSF) interface (nCSF≈1.37) and reflection at the PLGA–electrode interface; tip inclination of the waveguide is engineered (50–90°) to optimize emission into tissue aligned with electrode windows. The input cone angle (~19.5°) satisfies TIR criteria. Tip angle and electrode grid parameters (line width, fill factor) were optimized via experiments and ZEMAX OpticStudio ray-tracing (monochromatic, 1×10^7 rays) with quantitative image-based comparison and noise filtering. Fabrication: PLGA waveguides were formed using soft lithography from SU-8 master molds (including angled tip structures) replicated in PDMS. The Mo/Si electrode array was fabricated from an SOI wafer: solid-state P doping of top Si (300 nm), release of Si nanomembrane, layer transfer, Mo deposition by e-beam evaporation, photolithography and RIE for patterning, and sequential transfer processes to invert layer order (Mo beneath Si at recording surface). SiO2 encapsulation was deposited by PECVD; electrode windows were opened by wet etch (BOE). The electrode array was transfer-printed onto the PLGA waveguide using solvent-assisted adhesion; ACF cables were bonded to pads, and a fiber optic cannula (Ø105 µm core) was aligned and bonded with optical adhesive. Electrical/optical characterization: Electrochemical impedance spectroscopy (EIS) was performed in PBS (pH 7.4) using a three-electrode setup (Ag/AgCl reference, Pt counter) from 1 Hz–10 kHz at 10 mV AC, with Randles circuit fitting. Mechanical tests included bending on a 4 mm radius rod (up to 1000 cycles) and tensile testing of PLGA substrates. Accelerated degradation was performed in PBS pH 9.87 at 37 °C with periodic imaging. Visible transmittance (380–780 nm) of Si, Mo, and grid electrodes was measured by UV/Vis spectrophotometry. Photo-induced artifact evaluation: In vitro, electrodes (monolayer Si vs. Mo/Si) were placed in 0.7% agarose hydrogel. 460 nm laser pulses (100 ms, 2 Hz) with intensities 126.1–2522.5 mW mm^−2 were delivered; electrical signals were recorded (Intan RHD2000). In vivo artifact tests used adult wild-type mice (urethane anesthesia), with the device on somatosensory cortex; identical 460 nm pulses were delivered while recording ECoG on stimulation and control electrodes. Biocompatibility: Primary hippocampal neurons (rat E18) were cultured on control Au/PET and Mo/Si/PLGA electrodes; live/dead staining (AO/PI) and microscopy quantified viability. Immunohistochemistry assessed astrocytic (GFAP) and microglial (Iba-1) responses 2–8 weeks post-implantation; confocal imaging and ImageJ line-profile analysis compared ipsilateral vs. contralateral cortex. In vivo recording and optogenetics: Adult Thy-1:ChR2 transgenic mice underwent craniotomy (5 × 8 mm²). The bioresorbable hybrid device with head-stage, ACF cable, and optical cannula was implanted. Spontaneous ECoG and K-complexes under urethane anesthesia were recorded and compared to a contralateral Au electrode. Seizure-like activity was induced by pilocarpine. Optogenetic stimulation used 460 nm pulses (typical: 63.08 mW mm^−2 at tissue, 30 ms, 2 Hz) via the waveguide; evoked LFPs were recorded across channels over a 28-day period to assess chronic performance. Micro-CT tracked device dissolution over time. Temperature monitoring verified no hazardous heating during stimulation. Data acquisition used Intan hardware (notch 60 Hz, bandpass 1–300 Hz) and MATLAB for analysis. Statistical analyses included t-tests/ANOVA or Mann–Whitney as appropriate, reporting mean ± SEM.
Device performance and stability: EIS of electrodes fitted to a Randles model gave R_CT ≈ 902.9 MΩ and CPE ≈ 1.98 µF cm² (PBS). Bending (radius 4 mm) produced negligible impedance changes; after 1000 bending cycles, impedance changes were ~9.2% at 1 Hz and ~11.2% at 100 kHz (~10% across frequencies). Accelerated dissolution in PBS (pH 9.87, 37 °C) showed progressive exfoliation/dissolution of Mo, Si, SiO2, and hydrolysis of PLGA; in vivo, operational stability was maintained for ~3 weeks, after which SiO2 degradation restricted performance; complete dissolution occurred by ~8 weeks (traceable until day 21, absent by day 50 in micro-CT). Optical/electrode optimization: Grid-line width (40, 20, 10 µm; fill factor 56%) yielded transmittances at 460 nm of 49.0%, 49.4%, and 52.4% with impedances of 105.2, 105.6, and 107.6 kΩ at 1 kHz, respectively. Varying fill factor (63%, 56%, 42%; line width 20 or 10 µm as specified) produced 460 nm transmittances of 40.0%, 49.4%, and 60.4% and impedances of 98.4, 105.6, and 140.7 kΩ at 1 kHz. Corresponding Randles fits gave R_CT ≈ 568.9, 659.2, and 856.9 MΩ and CPE ≈ 3.14, 2.75, and 1.95 µF cm² for 63%, 56%, and 42% fill factors, respectively, confirming the fill factor as the dominant determinant of optical/electrical trade-offs. Ray-tracing and measurements indicated a 50° waveguide tip angle maximized delivered light intensity to tissue. Artifact suppression: Si nanomembranes (300 nm) transmitted ~30% of 460 nm light (≈70% absorption), while Mo (300 nm) blocked visible light, justifying the Mo anti-artifact layer. In agarose, monolayer Si electrodes exhibited pronounced photo-induced artifacts that scaled with light intensity (peaks ~400 µV to 3 mV from 126 to 2522 mW mm^−2) and saturated at high intensities; Mo/Si electrodes showed no discernible artifacts below ~630 mW mm^−2 and remained ≤200 µV even at 2522 mW mm^−2. In vivo in wild-type mice, Si stimulation electrodes showed ~400 µV artifacts and control sites ~50 µV due to scattering at 126 mW mm^−2, whereas Mo/Si electrodes showed no artifacts; at 2522 mW mm^−2, Mo/Si recorded ~200 µV artifact at the stimulated site attributable to tissue backscatter, with absent artifacts at control sites. Biocompatibility: Primary neuron cultures on Mo/Si/PLGA showed high viability comparable to Au/PET controls. Immunohistochemistry 8 weeks post-implantation revealed no significant differences in GFAP and Iba-1 intensities between ipsilateral (device) and contralateral hemispheres, indicating minimal glial activation. In vivo functionality: The device recorded spontaneous ECoG and K-complexes under urethane anesthesia comparable to Au controls. Pilocarpine-evoked seizure-like spiking was captured between 0–25 Hz. Optogenetic stimulation (460 nm, ~63.08 mW mm^−2, 30 ms, 2 Hz) evoked robust LFPs with peaks ~200–250 µV occurring ~15 ms after stimulation onset on day 0; responses scaled with intensity (≈100, 160, 230 µV for 15.77, 31.54, 63.08 mW mm^−2). Chronic recordings showed stable evoked LFPs for 14 days; by days 20–21, some channels failed (open-circuit from bioresorption) and waveguide erosion reduced transmitted light and LFP amplitudes (<150 µV); all channels failed by day 28. The implanted device fully disappeared by ~day 50.
The study demonstrates a fully bioresorbable, integrated opto-electronic neural interface that achieves selective optical stimulation with simultaneous electrophysiological recording, addressing challenges of mechanical mismatch, artifact contamination, and device removal. By combining a PLGA waveguide with a Mo/Si bilayer electrode and SiO2 encapsulation, the device maintains conformal cortical contact, optimizes optical delivery via tailored waveguide tip angles and electrode grids, and suppresses photoelectric artifacts through the opaque Mo layer shielding the Si recording surface. The system achieves artifact-minimized, reliable LFP recording during optogenetic stimulation, validates high biocompatibility in vitro and in vivo, and functions stably for over two weeks before controlled degradation leads to graceful end-of-life without surgical extraction. These results validate the feasibility of multifunctional transient neural implants for theranostic applications, enabling investigation of neural circuits and potential interventions (e.g., epilepsy) while mitigating long-term risks associated with permanent implants.
This work introduces and validates a fully bioresorbable hybrid opto-electronic neural implant that provides concurrent ECoG recording and optogenetic stimulation via a PLGA waveguide and Mo/Si bilayer electrodes engineered to minimize optical losses and photo-induced artifacts. The device exhibits robust mechanical stability, favorable optical/electrical trade-offs, biocompatibility, and stable in vivo operation for approximately two weeks, followed by complete resorption within about eight weeks. Key contributions include artifact suppression via a Mo anti-photovoltaic layer, waveguide/electrode co-design for efficient light delivery, and demonstration of chronic, simultaneous stimulation and recording without removal surgery. Future work should focus on precise control of biodegradation kinetics, increased channel counts and density, larger-area coverage, wireless power/communication integration, and scalable, cost-effective manufacturing to facilitate preclinical and clinical translation.
Operational lifetime is limited by bioresorption: insulation layer degradation restricts performance beyond ~3 weeks, with progressive channel failure by days 20–21 and complete loss by day 28; full dissolution occurs by ~8 weeks. Optical delivery incurs absorption losses at reflective interfaces (e.g., metal layer), reducing efficiency. Under very high optical intensities, residual artifacts can appear due to tissue backscatter even with the Mo/Si design. The current system involves tethered optical fibers and external acquisition (no wireless), and demonstrated channel counts (4–6) are modest relative to high-density arrays. Results are in mice; translational performance, long-term safety, and efficacy in larger brains remain to be established.
Related Publications
Explore these studies to deepen your understanding of the subject.