Medicine and Health
Examining differentials in HIV transmission risk behaviour and its associated factors among men in Southern African countries
M. Phiri, M. Lemba, et al.
This study explores the worrying variations in HIV risk behaviors among men in Southern Africa, highlighting the significant influences of education and other factors. Conducted by Million Phiri, Musonda Lemba, Chrispin Chomba, and Vincent Kanyamuna, the research calls attention to the urgent need for comprehensive sexuality education and targeted interventions to combat HIV regional challenges.
~3 min • Beginner • English
Introduction
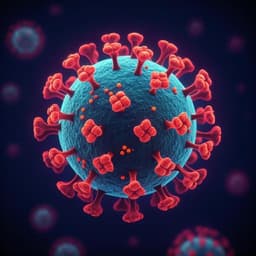
HIV/AIDS continues to have a substantial global burden, with sub-Saharan Africa (SSA) bearing over 70% of the global total of people living with HIV. In Southern Africa, HIV prevalence among males aged 15–59 is about 14%, and many countries have not reached epidemic control despite ART scale-up. Early studies in SSA suggested higher HIV risk among the more educated, but subsequent research indicated a reversal, with education conferring protective effects via improved knowledge and prevention behaviours. More recent evidence shows non-linear patterns, and findings remain mixed, underscoring the need for repeated population-level analyses. Given the persistently high HIV prevalence among men in Southern and Eastern Africa and limited regional evidence pooling men’s risk behaviours and associated factors, this study investigates individual-level and contextual determinants of HIV transmission risk behaviours among sexually active men in six Southern African countries. The study aims to quantify differentials and assess the role of education and other correlates in condom use, multiple sexual partnerships, and HIV testing, using comparable nationally representative DHS data to inform regional public health policy and programming.
Literature Review
Earlier epidemiological studies in SSA (late 1980s–early 1990s) reported formal education as a risk factor, with the educated more likely to acquire HIV. Later demographic research found a reversal, with education acting as a protective social factor by improving comprehensive knowledge and prevention strategy uptake. Some recent work indicates a curvilinear relationship between educational attainment and HIV risk. Studies also document associations between education and reduced HIV infection risk (e.g., natural experiments in Botswana), and show that schooling can be protective for young women in South Africa. Evidence links education to higher HIV testing uptake and better engagement in preventive behaviours, though heterogeneity across countries is noted. Concurrently, structural and behavioural drivers such as multiple partnerships, inconsistent condom use, socio-cultural norms (e.g., acceptance of polygamy, male decision-making dominance), residence, wealth, and employment have been implicated in HIV transmission dynamics. Programmatically, regional initiatives (PEPFAR, UNAIDS, Global Fund) promote abstinence for the unmarried, delayed sexual debut, monogamy, consistent condom use, and medical male circumcision; however, comprehensive regional analyses focusing on men’s behaviours remain limited.
Methodology
Data source and setting: The study used the most recent Demographic and Health Survey (DHS) men’s datasets from six Southern African countries: Lesotho, Mozambique, Namibia, South Africa, Zimbabwe, and Zambia. Surveys employ two-stage stratified cluster sampling and are weighted to account for complex design and response bias. Survey years reflected in analysis tables were Lesotho 2014, Mozambique 2011, Namibia 2013, South Africa 2016, Zimbabwe 2015, and Zambia 2018.
Sample: Men aged 15–59 years were included; only those sexually active at the time of survey were analyzed. The pooled unweighted sample was 29,533 men (weighted n=27,019). Country weighted samples of sexually active men ranged from 2,255 (Lesotho) to 9,224 (Zambia).
Outcome measures: Three binary outcomes were considered: (1) condom use during last sex with the most recent partner (0=non-use, 1=use); (2) multiple sexual partnerships (0=one partner, 1=two or more partners in reference period); (3) HIV testing in the last 12 months (0=no, 1=yes).
Independent variables: Individual and household correlates included age (15–24, 25–34, 35–44, 45–54, 55–59), marital status (never married, married/living with partner, formerly married), residence (urban/rural), education (none, primary, secondary, tertiary), literacy (illiterate/literate), household wealth index (recoded to poor, middle, rich), employment (no/yes), age at first sex (below 15, 15–24, 25+), and circumcision status (no/yes).
Statistical analysis: Analyses were conducted in Stata SE 17 using svy commands to account for complex survey design and weights. Descriptive statistics (percentages and counts) and country-specific cross-tabulations with chi-square tests examined bivariate associations. Multivariate binary logistic regression models were fitted on pooled and country-specific datasets to estimate adjusted odds ratios (AOR) and 95% confidence intervals for each outcome. Model choice reflected dichotomous outcomes and included all independent correlates identified in prior literature. Ethical considerations: DHS data access was granted by the DHS Program; original surveys received national and CDC ethical approvals, and the de-identified secondary data analysis required no additional approval.
Key Findings
Descriptives and bivariate patterns:
- Condom use during last sex with the most recent partner varied widely: 18.2% in Mozambique to 59.1% in Namibia. Condom use was generally higher among younger, urban, never-married, literate, and wealthier men. HIV prevalence among men 15–59 ranged from 8.3% (Zambia) to 19.6% (Lesotho), and was lower among men with secondary or higher education in most countries (exception noted in Zambia).
- Multiple sexual partnerships were least prevalent in Namibia (13.7%) and highest in Lesotho (32.9%). Younger age, earlier sexual debut, rural residence (in several countries), wealth, and never-married status were associated with higher prevalence.
- HIV testing in the last 12 months ranged from 23.0% (Mozambique) to 77.9% (Zambia). Testing was more common among older age groups, urban residents, married/formerly married men, those with higher education and literacy, wealthier households, and circumcised men in most countries (exception Mozambique).
Pooled multivariate results (AOR [95% CI]):
- Condom use: Older age associated with lower odds (e.g., 55–59 vs 15–24: AOR 0.63 [0.49–0.81]); rural residence lower (0.72 [0.66–0.78]); married (0.11 [0.10–0.12]) and formerly married (0.59 [0.50–0.69]) had lower odds than never married. Wealth increased odds (middle 1.25 [1.13–1.39]; rich 1.30 [1.19–1.42]); circumcision increased odds (1.17 [1.08–1.27]). Education was not significantly associated overall in pooled models.
- Multiple partnerships: Older age reduced odds (e.g., 55–59 vs 15–24: 0.45 [0.35–0.59]); rural residence increased odds (1.24 [1.13–1.36]); formerly married increased odds (1.25 [1.05–1.49]); later sexual debut reduced odds (15–24: 0.60 [0.55–0.66]; 25+: 0.22 [0.17–0.28]); wealth increased odds (middle 1.22 [1.10–1.35]; rich 1.36 [1.24–1.50]); circumcision increased odds (1.27 [1.17–1.37]). Education not associated.
- HIV testing: Older age increased odds (25–34: 2.04 [1.85–2.25]; 35–44: 2.13 [1.89–2.39]); rural residence reduced odds (0.83 [0.75–0.92]); married (1.51 [1.38–1.66]) and formerly married (1.36 [1.16–1.59]) higher than never married; education strongly increased odds (primary 1.44 [1.24–1.66]; secondary 3.10 [2.64–3.64]; higher 5.19 [4.18–6.45]); rich wealth increased odds (1.21 [1.10–1.34]). Employment and circumcision were not associated with testing in pooled models.
Country-level multivariate highlights:
- Condom use: Education significantly increased condom use only in Mozambique and Zimbabwe; older age reduced condom use in Lesotho, Mozambique, Namibia, and South Africa, while in Zimbabwe older men had higher odds than 15–24; rural residence reduced condom use in all countries except South Africa; wealth gradients were strong in Mozambique (middle AOR 2.79 [1.68–4.63]; rich 4.90 [2.93–8.20]).
- Multiple partnerships: Education not significantly associated in any country; later sexual debut consistently reduced odds of multiple partnerships.
- HIV testing: Education significantly increased testing in Lesotho, Mozambique, Namibia, Zimbabwe, and Zambia; mixed age effects by country; rural residence reduced testing odds in Lesotho; wealth increased testing in Mozambique (middle 1.73 [1.19–2.53]; rich 5.13 [3.64–7.25]) and in South Africa (rich 1.43 [1.09–1.88]); circumcision increased testing odds in all countries except Mozambique.
Discussion
The study addressed the research question by quantifying how education and other individual/household factors relate to HIV transmission risk behaviours among men across six Southern African countries. While pooled results did not show a significant association between education and condom use or multiple partnerships, education strongly and consistently increased HIV testing uptake, aligning with literature that links schooling to better health knowledge and preventive action. The analysis confirmed that age, marital status, residence, and wealth are important predictors: older men and those in rural areas are less likely to use condoms; never-married men report more multiple partnerships; and wealthier, urban men have higher condom use and testing rates. Later sexual debut substantially reduces the likelihood of multiple partnerships, underscoring the potential of comprehensive sexuality education and adolescence-focused interventions. Country-specific heterogeneity indicates that contextual factors shape the education–behaviour linkage: education was associated with condom use only in Mozambique and Zimbabwe, and rural-urban disparities in testing were not uniform. These findings suggest that regional strategies should be adapted to country contexts, strengthening targeted social and behaviour change communication (SBCC), expanding access to education, and addressing structural determinants (wealth, urbanicity). Enhancing community and school-based HIV testing initiatives, including self-testing, may be effective to boost uptake among men, particularly those with lower education.
Conclusion
Education is an important determinant of HIV testing uptake among sexually active men in Southern Africa, though its influence on other HIV risk behaviours (condom use, multiple partnerships) varies by country. Age, residence, marital status, wealth, and circumcision status were significantly associated with men’s HIV risk behaviours. Investing in education may be a cost-effective long-term intervention to improve testing uptake and reduce HIV infections among men in some settings. Given disparate outcomes of country-level prevention campaigns, programmes should be re-evaluated to identify best practices. Strengthening community SBCC to discourage multiple partnerships and integrating comprehensive sexuality education into primary and secondary school curricula could yield long-term reductions in men’s HIV risk behaviours. Further qualitative research is needed to elucidate socio-cultural reasons why educated men may still engage in risky behaviours such as multiple partnerships.
Limitations
The DHS data are cross-sectional, preventing causal inference and limiting understanding of men’s HIV risk behaviours across the life course. Additional qualitative and longitudinal studies are needed to unpack the interplay of individual and community factors. Although DHS male datasets provide rich behavioural information, data for some Southern African countries were unavailable on the DHS website, potentially limiting regional generalizability.
Related Publications
Explore these studies to deepen your understanding of the subject.