Veterinary Science
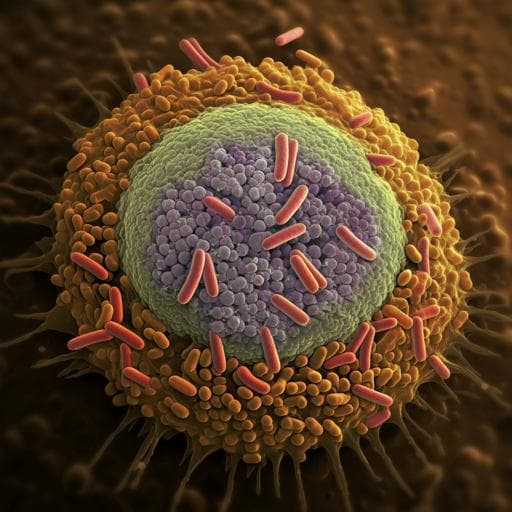
Epithelial processed *Mycobacterium avium* subsp. *paratuberculosis* induced prolonged Th17 response and suppression of phagocytic maturation in bovine peripheral blood mononuclear cells
H. Park, H. Park, et al.
Discover groundbreaking insights into Johne's disease as researchers, including Hong-Tae Park and his team, uncover how *Mycobacterium avium* subsp. *paratuberculosis* manipulates host immunity and lipid metabolism, leading to a prolonged Th17 response. This study reveals the complexities of host-MAP interactions through innovative transcriptomic analysis.
Related Publications
Explore these studies to deepen your understanding of the subject.