Medicine and Health
Dual role of Ca²⁺-activated Cl⁻ channel transmembrane member 16A in lipopolysaccharide-induced intestinal epithelial barrier dysfunction in vitro
J. Sui, C. Zhang, et al.
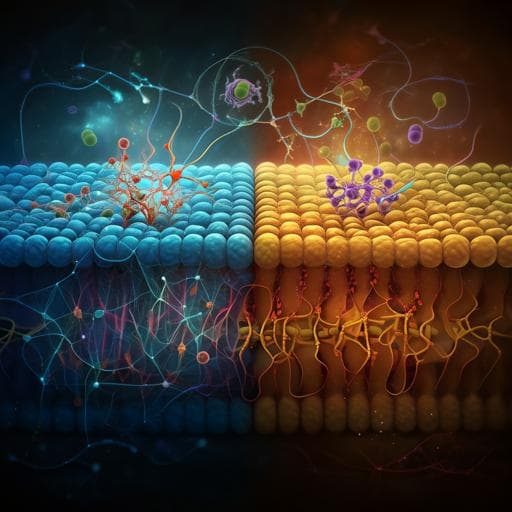
The intestinal epithelium forms a key biochemical and physical barrier that separates the host from the external environment and microbiota. Disruption of epithelial or immune homeostasis can lead to microbial translocation, inflammation, and diseases such as inflammatory bowel disease (IBD). Barrier integrity depends on multiple factors, including mucosal defenses (mucins, antimicrobial proteins, IgA), regulated epithelial apoptosis/proliferation, and intercellular junctions (tight and adherens junctions). Tight junctions largely determine paracellular permeability, but excessive epithelial apoptosis independently causes barrier dysfunction. TMEM16A (ANO1), a Ca²⁺-activated Cl⁻ channel identified in 2008, is expressed in intestinal epithelial cells and regulates apical Cl⁻ efflux and fluid transport. TMEM16A has been implicated in diverse diseases and diarrheal processes; however, its role in intestinal epithelium remains controversial, with reports supporting and refuting its involvement in Ca²⁺-activated anion transport and mucus homeostasis. TMEM16A can modulate inflammatory responses and apoptosis in other tissues. This study aimed to clarify TMEM16A expression and function in intestinal epithelial cells by examining its effects on apoptosis and tight junction barrier function in an in vitro LPS-induced barrier dysfunction model using IEC-6 cells.
Prior work has documented altered epithelial Cl⁻ secretion in intestinal inflammation and implicated TMEM16A as a mediator of Ca²⁺-activated Cl⁻ secretion in colonic epithelium. TMEM16A expression is upregulated by bacterial components and Th2 cytokines in airway disease and contributes to mucin secretion (notably MUC5AC/MUC5B) in the respiratory tract; in the gut, where MUC2 predominates, TMEM16A’s role is debated. Some studies suggest TMEM16A is essential for ATP-dependent mucus secretion in the intestine, whereas others report normal calcium-activated anion secretion and mucus homeostasis despite epithelial TMEM16A deletion. In murine DSS colitis, TMEM16A protein levels were reported decreased, potentially via cytokine-mediated mechanisms, but findings on expression and localization vary, with some claiming minimal detection in colon tissue. TMEM16A is highly expressed in several intestinal epithelial and immune cell lines in vitro (e.g., IEC-6, RAW264.7, Caco-2, MODE-K). Beyond the gut, TMEM16A influences inflammatory responses (e.g., attenuating LPS-induced inflammation in lung epithelia), fluid clearance, and cancer cell apoptosis, underscoring context-dependent functions.
Design: In vitro and in vivo studies were conducted. Primary focus was on an IEC-6 rat intestinal epithelial cell model of LPS-induced barrier dysfunction, complemented by mouse colitis models to assess in vivo TMEM16A expression.
Cell culture: IEC-6 cells were maintained in DMEM (4.5 mg/mL glucose) with penicillin/streptomycin, glutamine, HEPES, and 10% FBS at 37°C, 5% CO₂, grown to confluence to form monolayers. Transepithelial electrical resistance (TER) was measured using an epithelial voltohmmeter.
LPS treatments: Cells were exposed to LPS at 0.1, 1, or 10 µg/mL. Barrier dysfunction was assessed over 12–24 h via TER.
Genetic manipulations: Knockdown was performed using siRNAs targeting TMEM16A and NF-κB p65 (Dharmacon) transfected with Lipofectamine 3000; controls used non-targeting siRNA. Overexpression used an adenovirus expressing TMEM16A-GFP (AdCMV/TMEM16A-GFP). ERK pathway involvement was probed with siRNAs targeting ERK1 and ERK2. Knockdown/overexpression efficiency was confirmed by western blotting and/or immunofluorescence.
Molecular assays: TMEM16A mRNA levels were quantified by qRT-PCR (normalized to GAPDH). Protein expression (TMEM16A, p-ERK1/2, ERK1/2, ELK-1, MLCK, cleaved caspase-3, Bcl-2, Bax) was analyzed by SDS-PAGE and western blot with chemiluminescent detection and densitometry. Immunofluorescence was used to visualize TMEM16A and other markers (with DAPI nuclear counterstain) via confocal microscopy.
Apoptosis assays: After 12 h incubation with 10 µg/mL LPS (under TMEM16A knockdown or overexpression), apoptosis was quantified using Annexin V-FITC/PI staining and flow cytometry. Apoptotic cells were defined as Annexin V-positive/PI-negative. Apoptosis-related proteins were evaluated by western blot. Cell proliferation was assessed by CCK-8 and BrdU incorporation; MTT is also mentioned for viability; a proliferation/apoptosis ratio was derived across time points (0–72 h) under LPS.
Pathway interrogation: Effects of TMEM16A manipulation on ERK1/2 activation and downstream ELK-1 and MLCK were assessed under low-dose LPS (0.1 µg/mL) to probe tight junction regulation. ERK1 and ERK2 knockdowns were used to determine their contributions to MLCK expression and barrier effects.
In vivo colitis models: Male C57BL/6 mice were used under approved protocols. DSS colitis: 2.5% DSS in drinking water for 7 days; tissues harvested at days 3 and 7. TNBS colitis: single intracolonic dose 125 mg/kg in 50% ethanol; distal colon harvested at days 7 and 14. Colonic epithelium was analyzed by H&E for histology and by immunofluorescence, qRT-PCR, and western blot for TMEM16A expression.
Statistics: Single-blind design; data presented as mean ± SD; comparisons by one-way ANOVA for ≥3 groups or Student’s t-test for two groups; non-parametric Kruskal–Wallis as needed. n typically 3–6/group; significance set at p<0.05.
- LPS upregulates TMEM16A: In IEC-6 cells, LPS at 0.1, 1, and 10 µg/mL significantly increased TMEM16A mRNA and protein; similar protein upregulation occurred in RAW264.7 macrophages. NF-κB p65 knockdown significantly attenuated the 10 µg/mL LPS-induced TMEM16A increase, implicating NF-κB in transcriptional regulation.
- Barrier function (TER): LPS (0.1, 1, 10 µg/mL) for 24 h reduced TER, indicating barrier dysfunction. TMEM16A manipulation exerted dose-dependent, opposite effects: • Low-dose LPS (0.1–1 µg/mL): TMEM16A overexpression further decreased TER (aggravating dysfunction), while TMEM16A knockdown mitigated TER loss. • High-dose LPS (10 µg/mL): TMEM16A overexpression improved TER (protective), while TMEM16A knockdown worsened TER loss.
- Tight junction regulation under low-dose LPS: Low-dose LPS increased MLCK expression. TMEM16A knockdown reduced p-ERK1/2, ELK-1, and MLCK, whereas TMEM16A overexpression increased ERK1/2 activation and MLCK. ERK1 or ERK2 knockdown reduced MLCK, and ERK1 knockdown attenuated the TMEM16A overexpression-induced MLCK increase. These findings support a TMEM16A→ERK1/ELK-1→MLCK axis leading to tight junction dysregulation and barrier loss at low-dose LPS.
- Apoptosis under high-dose LPS: High-dose LPS (10 µg/mL) increased apoptosis (Annexin V+/PI−) and elevated cleaved caspase-3 and Bax while reducing Bcl-2. TMEM16A overexpression decreased apoptosis (lower cleaved caspase-3 and Bax, higher Bcl-2), whereas TMEM16A knockdown increased apoptosis markers, consistent with a protective anti-apoptotic effect mediated via ERK1/2 signaling.
- Proliferation/apoptosis balance: Under low-dose LPS, overexpression of TMEM16A increased the proliferation/apoptosis ratio from 24–72 h; under high-dose LPS, TMEM16A overexpression attenuated the decrease in this ratio, linking TMEM16A to enhanced survival/proliferation in stress.
- In vivo expression: In DSS colitis, colonic epithelial TMEM16A mRNA and protein were significantly decreased at days 3 and 7 versus sham. In TNBS colitis, TMEM16A increased at day 7 and decreased at day 14. Immunofluorescence showed low baseline TMEM16A protein expression in colonic epithelium, more readily detected in distal colon. Overall, TMEM16A exhibits a dual role in LPS-induced barrier dysfunction: deleterious via tight junction dysregulation at low-dose LPS (ERK1/ELK-1/MLCK pathway) and protective via anti-apoptotic ERK/Bcl-2/Bax signaling at high-dose LPS.
The study addressed whether TMEM16A contributes to intestinal epithelial barrier dysfunction and how its role depends on inflammatory intensity. LPS robustly induced TMEM16A via an NF-κB–dependent mechanism. Functionally, TMEM16A exacerbated barrier leak in low-grade inflammatory conditions (low-dose LPS) by activating ERK1/ELK-1 and upregulating MLCK, a key mediator of tight junction opening, thereby worsening paracellular permeability. Conversely, during severe inflammatory stress (high-dose LPS), TMEM16A activation of ERK1/2 promoted anti-apoptotic signaling (increased Bcl-2, decreased Bax and cleaved caspase-3), preserving epithelial integrity and TER. These context-dependent effects reconcile disparate observations in the literature about TMEM16A in intestinal physiology and inflammation. The in vivo findings that TMEM16A expression dynamically changes in DSS and TNBS colitis support the notion that its role evolves across disease stages. Collectively, the results suggest TMEM16A may initially promote permeability during early/mild inflammation but confer cytoprotection against apoptosis during severe inflammation. Understanding and temporally targeting TMEM16A and its downstream ERK pathways could provide therapeutic leverage to modulate barrier function in intestinal inflammatory diseases.
TMEM16A expression is upregulated by LPS in intestinal epithelial cells via NF-κB and exerts a dual, dose-dependent role in barrier dysfunction: it aggravates low-dose LPS-induced tight junction dysfunction through the ERK1/ELK-1/MLCK pathway, but protects against high-dose LPS-induced apoptosis via ERK1/2-mediated regulation of Bcl-2/Bax and caspase-3. In vivo, TMEM16A expression in colonic epithelium is dynamically regulated during DSS- and TNBS-induced colitis. These findings highlight TMEM16A as a context-dependent regulator of epithelial barrier integrity and a potential therapeutic target. Future work should delineate the temporal contribution of tight junction regulation versus apoptosis across disease stages, evaluate TMEM16A’s channel activity versus scaffolding roles, and test TMEM16A-targeted interventions in vivo in IBD models.
- The primary findings are from an in vitro IEC-6 model; in vivo functional validation of barrier outcomes was limited to expression analyses in colitis models without direct barrier measurements.
- The study focused on TMEM16A expression and downstream signaling; channel activity per se was not directly linked to barrier outcomes (prior data suggest channel inhibition did not affect proliferation/barrier in this context).
- TER and molecular assays were conducted over relatively short time frames; longer-term adaptation and additional signaling pathways may contribute.
- Potential confounders present in vivo (microbiota, mucus layer dynamics, immune cell interactions) were not modeled in vitro, limiting generalizability.
- Some assays reported small group sizes (n=3–6), and quantitative data were often normalized to control without absolute effect sizes reported.
Related Publications
Explore these studies to deepen your understanding of the subject.