Medicine and Health
Directed self-assembly of a xenogeneic vascularized endocrine pancreas for type 1 diabetes
A. Citro, A. Neroni, et al.
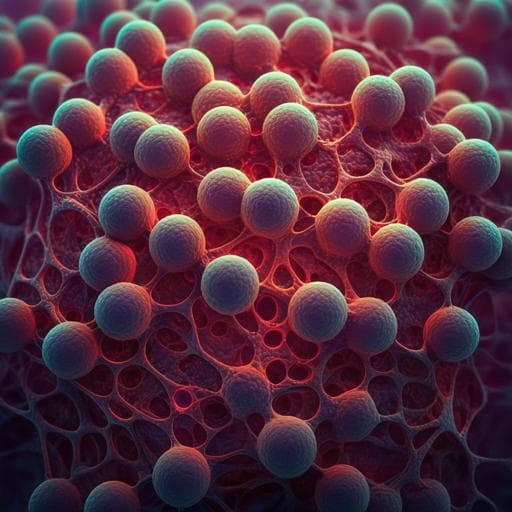
This groundbreaking research proposes using decellularized lungs as scaffolds for xenogeneic vascularized endocrine pancreas engineering, combining neonatal porcine islets with human endothelial cells. Conducted by a team from the San Raffaele Diabetes Research Institute in Milan, this study reveals promising results in islet maturation and sustained normoglycemia, paving the way for advanced diabetes treatments.
~3 min • Beginner • English
Introduction
Type 1 diabetes (T1D) is primarily managed by glucose monitoring and exogenous insulin therapy, which do not fully recapitulate dynamic islet-mediated glucose homeostasis and are burdened by compliance and complications. β cell replacement via islet or pancreas transplantation is limited by organ scarcity and immune rejection despite advances in immunosuppression. An alternative strategy requires (i) a sustainable, scalable source of endocrine cells and (ii) a scaffold that supports engraftment and physiological function while potentially reducing immunogenicity. Pigs are favored as a xenogeneic islet source due to insulin compatibility with humans, high fecundity, pathogen-free husbandry, and amenability to gene editing to reduce rejection and zoonosis. Neonatal porcine islets (NPIs) are readily isolatable and scalable but are immature, having only 10–20% of adult insulin content and requiring maturation. The microenvironment, including extracellular matrix (ECM) composition, geometry, and stiffness, critically regulates cell behavior and maturation. Prior studies demonstrated decellularized lung as a scaffold providing a dedicated vascular bed and native ECM that dramatically improve β cell survival, function, and in vivo performance. The present work tests whether a decellularized lung scaffold combined with human BOECs can direct the self-assembly of a vascularized endocrine organ from immature NPIs, enabling ex vivo maturation and superior in vivo engraftment and function.
Literature Review
- Donor shortage and immune rejection limit clinical β cell replacement via islet/pancreas transplantation.
- Xenogeneic sources: Porcine islets are attractive due to biological compatibility, breeding advantages, designated pathogen-free maintenance, and gene-editing tools addressing rejection, function, and zoonosis.
- NPIs are scalable but immature, needing maturation protocols and supportive ECM; prior approaches with native or synthetic ECM improved maturation but failed to achieve immediate orchestrated function.
- ECM biophysical and biochemical cues direct differentiation and function; decellularized organ ECM has shown promise for β cell engraftment and performance.
- Decellularized lung scaffolds previously improved islet survival and function by providing native vascular access and ECM.
- BOECs are an accessible autologous endothelial source with high proliferative capacity and in vivo neovascularization potential, proposed in gene therapy and hemophilia, supporting their use to build a biocompatible vascular bed.
- Prevascularization and neurovascular integration are critical determinants of islet graft success; device-less subcutaneous approaches can work for mature islets/human cells but may be insufficient for immature NPIs requiring high metabolic support.
Methodology
- Scaffold preparation: Decellularized left lung lobes from male Lewis rats prepared by vascular-detergent perfusion (SDS, Triton X-100), extensive washing, and quality control for infection/air trapping/leakage.
- Endothelial cell source and characterization: Human BOECs isolated from peripheral blood of healthy donors under ethical approvals; cultured and expanded. Phenotype confirmed by immunofluorescence (CD31, vWF, VE-cadherin, VEGFR2) and flow cytometry (CD31, VE-cadherin, KDR; CD34 negative). BOEC proliferation assessed by WST-1 under standard BOEC medium (BCM) vs VEP media. Tube formation assay on Matrigel comparing BCM, angiogenic medium (AM), modified stabilization medium (MSM), and the two-phase VEP media combination.
- Endocrine cell source: NPIs (WT and iRFP transgenic) isolated from 1–7-day-old piglets by collagenase digestion and cultured in recovery then maturation media. iRFP signal confirmed for tracking.
- VEP assembly and culture: Decellularized lungs mounted in custom bioreactor; BOECs seeded via pulmonary artery and vein (gravity, then perfusion). Next day, NPIs plus BOECs seeded via trachea into the airspace. Culture 7 days: 5 days AM then 2 days MSM. Controls included VEPs without BOECs (VEP-BOEC−) seeded with NPIs (7 or 21 days in vitro matured for specific experiments). Spatial organization assessed by immunofluorescence; perfusability tested by fluorescence microangiography with 0.2 μm microspheres.
- Endocrine maturation assays: mRNA (ddPCR) for pig insulin, glucagon, somatostatin normalized to cell content; protein by immunofluorescence at day 1 vs day 7; fluorescence quantification blinded.
- Functional testing ex vivo: Dynamic insulin secretion tests (perifusion) on NPIs in standard culture vs NPIs in VEP at day 7; parameters included point-by-point insulin levels, biphasic secretion (first phase min 2–5, second phase min 5–8), and AUC. Also compared VEPs at day 7 vs day 14 and VEP vs VEP-BOEC−.
- β cell death tracking: miR-375 quantification in VEP supernatants over 7 days by ddPCR; controls with BOEC-only VEPs; conversion of copies to percent β cell death using per-cell estimates.
- In vivo studies: Severe diabetes induced in NSG mice by alloxan. Transplanted groups: VEPs (subcutaneous, two segments), NPIs into device-less prevascularized subcutaneous pouch (DL-NPIs), under kidney capsule (KC-NPIs), or intrahepatically via portal vein (LV-NPIs; 800 NPIs due to surgical limits). Follow-up: DL/LV 9 weeks; KC 14–18 weeks; VEPs up to 18 weeks. Non-fasting glycemia monitored; Kaplan–Meier for normoglycemia; OGTT at 9 weeks; explantation to confirm graft dependence. iRFP imaging (IVIS) pre- and post-implant; spectral unmixing to confirm signal.
- Vascularization and innervation analyses: Gross pathology and AngioTool analysis of vessel density at 1, 2, 4, 9, 14, and 18 weeks; immunofluorescence for human/mouse endothelium; TEM at 14 weeks; neural markers at later timepoints.
- Statistics: Mann–Whitney U, Student’s t-tests, ANOVA with corrections, general linear model repeated measures with Bonferroni, log-rank for Kaplan–Meier; significance p<0.05.
Key Findings
- BOECs retained endothelial phenotype (CD31, vWF, VE-cadherin, VEGFR2; CD34−) and showed enhanced proliferation in VEP media vs BCM at 24 and 48 h (WST-1: p=0.0002 for both times). VEP media combination improved tube formation vs BCM (Mean Mesh size: p=0.0235).
- Directed self-assembly in decellularized lung produced a continuous human endothelial network with insulin+ NPIs integrated within the BOEC vascular bed by day 7; microangiography confirmed a perfusable vascular architecture.
- Endocrine maturation: Day 7 VEPs had significantly increased insulin staining with preserved glucagon and somatostatin vs day 1; mRNA increased 3.5-fold (insulin), 1.1-fold (glucagon), 1.9-fold (somatostatin) at day 7 vs day 1. NPIs in VEP showed higher insulin and glucagon fluorescence than batch-matched NPIs in standard culture at day 1 and 7.
- Functional secretion: At 20 mM glucose, VEPs displayed robust biphasic insulin secretion; NPIs in standard culture did not. Point-by-point insulin release higher in VEPs (min 2 p=0.026; min 3 p<0.0001; min 4 p=0.0002; min 5 p=0.0155; min 7 p=0.0085). First-phase peak at min 3: VEP 2.02±0.43 vs NPIs 0.89±0.03 fold-change (p<0.0001). Second-phase at min 7: VEP 1.27±0.3 vs NPIs 0.74±0.32 fold-change (p=0.0085). AUC: VEP first phase 3.43±0.9 vs NPIs 1.6±0.2 (p<0.0001); second phase 2.37±0.5 vs 1.43±0.5 (p=0.0031). Biphasic kinetics preserved at day 14 with trend to increased insulin production.
- Role of endothelium: VEP without BOECs (VEP-BOEC−) showed reduced in vitro functional maturation at day 7 (e.g., min 3 p=0.009; min 4 p=0.0157) and in vivo delayed normoglycemia by 4 weeks, indicating endothelial cells are key for maturation and engraftment.
- β cell survival: miR-375 release kinetics indicated low β cell death (0–5%) over 7-day VEP maturation; BOEC-only controls showed no miR-375.
- In vivo efficacy: VEPs outperformed DL-, KC-, and LV-NPIs with significantly lower non-fasting glycemia over follow-up (VEP vs DL p=4.98e-39; vs KC p=3.85e-29; vs LV p=2.01e-25). Higher proportion reached normoglycemia earlier (Kaplan–Meier: VEP vs DL p=1.2e-05; vs KC p=1.2e-05; vs LV p=0.00074). OGTT at 9 weeks showed improved glucose handling for VEPs (AUC comparison p=0.0463). Explantation of VEPs reversed normoglycemia, confirming graft dependency.
- Graft integration: Progressive vascularization of VEP surface over time (AngioTool vessel density: 12.53±3.58% at 2/4 weeks vs 32.26±5.78% at 14 weeks and 36.37±2.37% at 18 weeks; p<0.0001). Human and murine endothelium coexisted within graft; TEM at 14 weeks showed perfused capillaries with RBCs and nerve structures near endocrine cells. No immune infiltrates detected in NSG recipients at 9 weeks.
- Site comparisons: KC-NPIs reversed diabetes within ~8 weeks (consistent with literature), while LV-NPIs showed a similar trend despite an eightfold lower implanted mass, emphasizing vascular connection over mass. Device-less subcutaneous NPIs failed to reverse diabetes here, underscoring VEP advantages in hypoxic subcutaneous environments.
Discussion
The study addresses the critical need for an unlimited β cell source and a supportive scaffold enabling fast, durable function. By leveraging decellularized lung ECM and autologous-compatible BOECs, the VEP platform provides a pre-formed perfusable vascular bed that accelerates NPI maturation and engraftment. Data show enhanced endocrine marker expression, physiological biphasic insulin secretion, low β cell death during ex vivo maturation, and immediate, sustained glycemic control post-implantation for up to 18 weeks—superior to standard transplantation sites. Endothelial cells are central to both ex vivo maturation and in vivo engraftment, highlighting the importance of a vascularized ECM microenvironment. Progressive vascularization and innervation of the graft likely underpin long-term performance. These findings suggest that combining gene-edited porcine endocrine tissues with patient-derived BOECs in a decellularized scaffold could yield immune-compatible, functional endocrine organs, advancing β cell replacement strategies for T1D.
Conclusion
This work demonstrates a directed self-assembly approach to engineer a xenogeneic vascularized endocrine pancreas from immature NPIs and human BOECs within a decellularized lung scaffold. The VEP promotes ex vivo endocrine maturation, preserves β cell mass, and achieves immediate and durable glycemic control after subcutaneous implantation, outperforming conventional transplantation sites. The platform’s native ECM and compartmentalized architecture support ex vivo engraftment and integration of endocrine and endothelial components and can be tailored by matrix modifications. Future efforts should focus on clinical-grade manufacturing, further characterization of nutrient exchange (e.g., vessel fenestration), and combining gene-edited pig islets/organs with autologous BOECs to minimize immune rejection and enable translation to T1D therapy.
Limitations
- In vivo studies were conducted in immunodeficient NSG mice; immune compatibility and rejection were not assessed.
- Electron microscopy did not observe vessel fenestration, though functional exchange was inferred from glycemic control.
- Liver transplantation was limited by a reduced NPI mass due to surgical constraints, complicating direct comparisons of dose-response.
- BOEC isolation efficiency can vary by donor colony-forming capacity, potentially impacting scalability.
- miR-375, while useful for β cell death tracking, can originate from multiple cell types in vivo; here specificity was addressed by using BOEC-only controls but broader applicability may still be constrained.
Related Publications
Explore these studies to deepen your understanding of the subject.