Medicine and Health
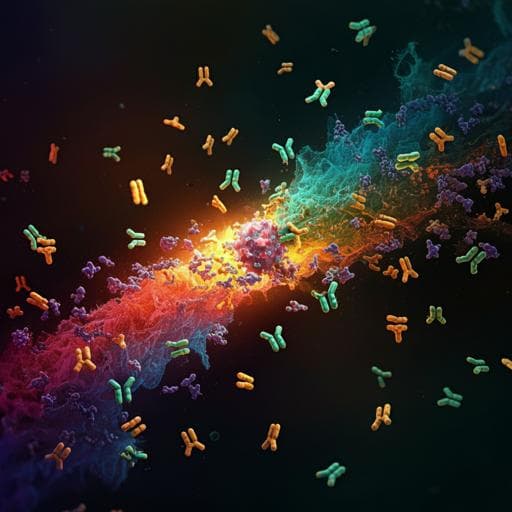
COVID-19 vaccination boosts the potency and breadth of the immune response against SARS-CoV-2 among recovered patients in Wuhan
H. Liang, X. Nian, et al.
This study reveals how inactivated COVID-19 vaccines can significantly enhance the immune response in recovered patients, boosting both humoral and cellular immunity against variants like Delta and Omicron for up to nine months. Conducted by renowned researchers including Hong Liang and Xuanxuan Nian, this work highlights the ongoing importance of vaccination in the face of evolving viruses.
Related Publications
Explore these studies to deepen your understanding of the subject.