Medicine and Health
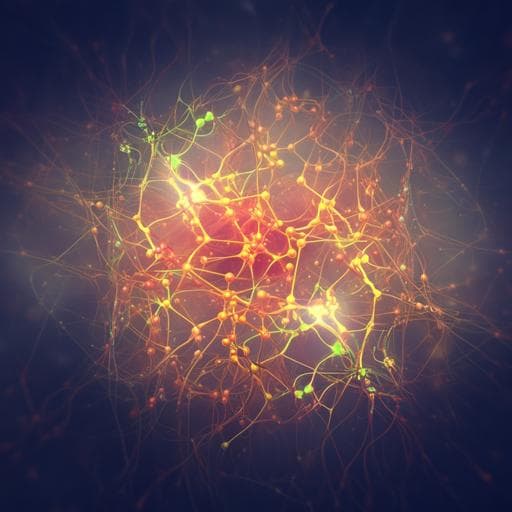
Cortical structure and the risk for Alzheimer’s disease: a bidirectional Mendelian randomization study
B. Wu, Y. Zhang, et al.
This groundbreaking study by Bang-Sheng Wu and colleagues explores the intriguing link between brain structure and Alzheimer's disease risk. It reveals suggestive associations of cortical surface area alterations, exciting the field with potential new insights into vulnerability factors for AD.
Related Publications
Explore these studies to deepen your understanding of the subject.