Medicine and Health
Cell-based versus corticosteroid injections for knee pain in osteoarthritis: a randomized phase 3 trial
K. Mautner, M. Gottschalk, et al.
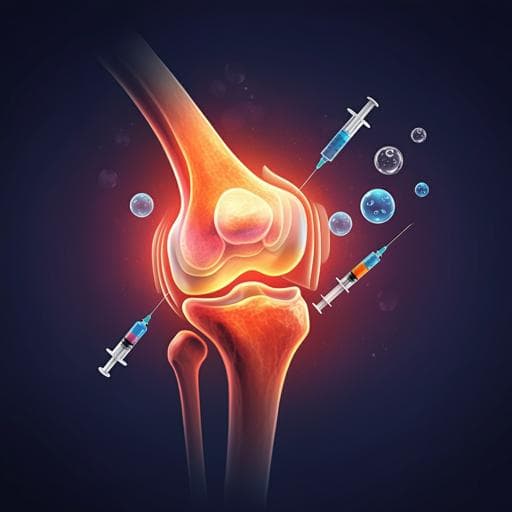
Osteoarthritis (OA) is a prevalent, degenerative joint disease affecting over 54 million Americans and imposing substantial economic burden. Despite advances in symptomatic management, a disease-modifying therapy has remained elusive. Mesenchymal stromal/stem cell (MSC) injections are increasingly used in orthopedics to reduce pain and improve function, but high-quality randomized controlled trials comparing cellular therapies with standard treatments are limited. This study aimed to determine the safety and efficacy of three cellular injectates—autologous bone marrow aspirate concentrate (BMAC), autologous adipose stromal vascular fraction (SVF), and allogeneic umbilical cord tissue-derived mesenchymal stromal cells (UCT)—compared with corticosteroid injection (CSI) for knee OA. The co-primary outcomes were change from baseline to 12 months in VAS pain and KOOS pain. The hypothesis was that cell therapies would be superior to corticosteroids at 1 year.
The orthopedic and broader clinical literature has explored MSC therapies for chronic diseases, including OA, citing potential anti-inflammatory and chondroprotective mechanisms. However, clinical data supporting injectable cellular therapies are heterogeneous, with limited well-designed randomized trials. Prior rigorous trials have sometimes shown no advantage of cellular products over controls; for example, a randomized study reported similar pain improvements in knees injected with BMAC versus saline. Conversely, case reports, series, and meta-analyses have reported favorable outcomes with MSC-based treatments. There is notable heterogeneity in autologous and allogeneic products due to donor variability and processing, and concerns exist regarding commercially available birth tissue products lacking viable MSCs. Autologous same-day procedures generally show high viability and good safety profiles, but consistent clinical efficacy has not been firmly established.
Design: Phase 2/3, multicenter, single-blind, randomized, controlled, four-cohort parallel study conducted under FDA oversight (IND #18414; IDE #17894) and registered at ClinicalTrials.gov (NCT03818737). Five US clinical sites (Emory, Sanford [two sites], Andrews Institute, Duke). IRB approvals obtained. Participants: 570 screened; 480 eligible randomized (ages 40–70; knee OA Kellgren–Lawrence II–IV). Randomization stratified by center with permuted blocks via Medidata Rave. Subjects blinded to treatment through opaque syringe coverings and sham harvests; investigators not required to be blinded. Arms and allocation: Three cellular cohorts each with its own CSI control, randomized 3:1 within cohort: Arm 1—BMAC (n=120) vs CSI (n=40); Arm 2—SVF (n=120) vs CSI (n=40); Arm 3—UCT (n=120) vs CSI (n=40). For analyses, CSI groups were aggregated to allow 1:1:1 comparisons with BMAC, SVF, and UCT. Interventions and procedures: Standardized across sites. If effusion present, local anesthetic administered and joint aspirated under ultrasound guidance. Injectate (CSI, BMAC, SVF, or UCT) delivered intra-articularly under ultrasound guidance. Post-injection passive knee motion and brief supine rest performed. BMAC and SVF were fresh autologous products; UCT consisted of cryopreserved, purified allogeneic MSCs manufactured in a cGMP facility. Point-of-care testing of cellular products included total nucleated cell count, cell viability, endotoxin testing; products failing release criteria were not injected (1 BMAC, 4 SVF). Fourteen-day sterility testing performed post administration. Follow-up and outcomes: MRIs at baseline, 6 months, and 12 months. Co-primary endpoints: change from baseline to 12 months in VAS pain and KOOS pain. Secondary endpoints: EQ-5D and PROMIS-29 domain scores. MRI evaluated with a semi-quantitative whole-joint scoring system adapted from WORMS and BLOKS; T2 mapping acquired in weight-bearing regions; MRI 0–69 composite score (higher = worse) used. Exploratory analyses included bedside total nucleated cell counts/viability and single-cell RNA sequencing of subsets of BMAC (n=71), SVF (n=16), and UCT-MSC (n=8) products to profile cellular composition. Statistical analysis: Primary analyses by intention-to-treat. Missing VAS and KOOS data imputed using multiple imputation under missing at random. Sensitivity analyses included observed case, per-protocol, and pattern-mixture multiple imputation under missing not at random. Repeated-measures means model (SAS MIXED, compound-symmetric covariance, robust SEs) with fixed effects for treatment, time (1, 3, 6, 9, 12 months), treatment-by-time interaction, and study center. Main effect at 12 months used for primary hypothesis tests; pairwise comparisons of each cellular group versus CSI with Hochberg multiplicity adjustment. Prespecified subgroup interactions tested for sex, ethnicity, and KL grade; additional analyses for age group (<60 vs ≥60). Secondary endpoints analyzed as observed cases with similar modeling. No interim efficacy analyses. Safety captured per FDA requirements; AEs summarized by MedDRA terms. Participants received $50 per MRI.
- Enrollment and demographics: 480 randomized; safety population n=440 treated. Mean age 58.3 years; mean BMI 30.8 kg/m^2; 45% male.
- Primary outcomes at 12 months showed no significant differences between any cellular therapy and CSI: • VAS pain change from baseline (model-based mean ± s.e.m.): BMAC -24.3, SVF -19.4, UCT -20.1, CSI -20.9. Differences vs CSI: BMAC -3.4 (P=0.19), SVF 1.5 (P=0.56), UCT 0.8 (P=0.76). • KOOS pain change from baseline (± s.e.m.): BMAC 19.1, SVF 17.2, UCT 16.2, CSI 17.7. Differences vs CSI: BMAC 1.4 (P=0.49), SVF -0.50 (P=0.82), UCT -1.5 (P=0.44). • All treatments exceeded minimally clinically important differences and sustained improvements to 12 months, but without between-group superiority. • Sensitivity analyses (observed case, per protocol, MNAR imputation) confirmed no significant between-group differences for VAS or KOOS. • Interaction tests: Significant interactions for VAS with age group (P=0.02) and sex (P=0.01); no significant interactions for KOOS.
- MRI outcomes: No significant within-group changes from baseline and no significant differences versus CSI in MRI composite scores (approximate mean changes: BMAC 0.53, SVF -0.40, UCT -0.26, CSI 0.30; between-group differences vs CSI: BMAC 0.23, SVF -0.69, UCT -0.55).
- Secondary outcomes: EQ-5D treatment-by-time interaction not significant (P=0.26). PROMIS-29 domain interactions not significant except Physical Function (P=0.048) with differing temporal patterns but no clear clinically important differences.
- Exploratory cellular analyses: scRNA-seq revealed distinct subpopulations in autologous BMAC and SVF with some shared hematopoietic-lineage similarities; UCT showed a more uniform MSC phenotype.
- Safety: No procedure-related serious adverse events or symptomatic infections. Significant differences in some related AEs: joint swelling higher with UCT vs CSI (24.1% vs 7.4%, P=0.01); post-procedural contusion more frequent with SVF vs BMAC vs UCT/CSI (38.6% vs 12.2% vs 0%, P<0.0001); post-procedural hematoma higher with SVF vs BMAC (12.4% vs 2.9%, P=0.02). Most AEs were mild and resolved by 1-week follow-up.
The trial directly tested whether commonly used orthobiologic cellular injections outperform corticosteroid injections in knee OA over 12 months. Despite clinically meaningful improvements across all groups, no cellular product (BMAC, SVF, UCT) demonstrated superiority to CSI on pain outcomes (VAS, KOOS), and MRI measures did not improve relative to CSI. The findings challenge assumptions that more costly cellular therapies provide superior 1-year benefit over standard corticosteroids in broad OA populations. Safety was favorable across all interventions, aligning with prior reports of low serious AE rates with autologous procedures. Subgroup analyses did not identify consistent predictors of superior response (KL grade was not a reliable predictor; some interaction signals for VAS by age and sex did not translate to KOOS). The lack of MRI change may reflect OA’s slow progression and a 1-year horizon being too short to detect structural modification. Placebo effects and procedural factors complicate interpretation in OA injection trials; however, blinding and sham procedures were implemented to mitigate bias. Overall, results suggest that while patients can achieve symptomatic improvement after injection, the choice among these cellular products versus CSI may not substantially alter 1-year pain outcomes, emphasizing safety, cost, and patient selection considerations.
In this large, multicenter, single-blind randomized controlled trial, none of the three cellular therapies (BMAC, SVF, UCT) was superior to corticosteroid injection for knee OA at 12 months on VAS and KOOS pain outcomes, and no MRI advantages were observed. All interventions showed clinically meaningful improvements and favorable safety profiles without procedure-related serious AEs. These findings inform clinicians and patients that, at 1 year, orthobiologic injections evaluated here do not confer superior symptom relief compared to CSI. Future work will include longer-term follow-up (2–3 years), deeper responder and subgroup analyses, and further characterization of MRI changes and cellular product heterogeneity to identify potential patient subsets or longer-term structural effects.
- Single-blind design: investigators were not required to be blinded, introducing potential bias.
- Potential selection bias between participants who initiated the trial and those who did not.
- Placebo and procedural effects are substantial in OA injection studies and difficult to fully disentangle, even with sham procedures.
- Insufficient racial diversity to conduct planned subgroup analyses by race/ethnicity.
- One-year follow-up may be too short to detect structural changes on MRI in a slowly progressive disease.
- Heterogeneity of autologous and allogeneic cell products and donor variability may affect generalizability and mask differential effects.
- No personalized treatment insights emerged despite exploratory analyses; interactions observed for VAS by age and sex were not consistent across outcomes.
Related Publications
Explore these studies to deepen your understanding of the subject.