Medicine and Health
An intranasal influenza virus-vectored vaccine prevents SARS-CoV-2 replication in respiratory tissues of mice and hamsters
S. Deng, Y. Liu, et al.
The emergence of SARS-CoV-2 and ongoing circulation of variants with immune-evasion capabilities have challenged efforts to end the COVID-19 pandemic. While current intramuscular mRNA, inactivated, subunit, and adenoviral vector vaccines induce strong systemic immunity that reduces severe disease and mortality, their ability to prevent infection in the upper respiratory tract is limited. Frequent breakthrough infections and reinfections suggest that strategies enhancing mucosal immunity are needed to reduce transmission. Intranasal vaccines have shown advantages in inducing local respiratory immunity in preclinical studies. Given the likelihood that SARS-CoV-2 will co-circulate with seasonal influenza, a dual-function vaccine could be advantageous. The authors previously developed NS1-deleted live-attenuated influenza viruses (DelNS1 LAIV) and versions expressing the SARS-CoV-2 spike RBD, showing safety in early clinical trials and immunogenicity in preclinical models. This study evaluates an improved LAIV candidate, DelNS1-RBD-DAF, engineered to express RBD on the cell surface and to focus responses on the ACE2-binding region via targeted N-glycosylation, assessing its immunogenicity and protective efficacy against contemporary variants in mice and hamsters, and benchmarking against BNT162b2 mRNA vaccination.
The paper situates its work within evidence that intramuscular COVID-19 vaccines protect against severe disease but have limited impact on upper airway infection. Several intranasal candidates have demonstrated strong mucosal immunity in animals. Prior work by the authors established NS1-deleted influenza vectors (DelNS1) as live-attenuated platforms and earlier DelNS1-RBD constructs were safe in phase I/II trials, eliciting RBD-directed antibody and T-cell responses, though airway-specific responses were not fully quantified. Background literature highlights Omicron subvariants’ antibody evasion, preservation of T-cell cross-reactivity to variants, and the public health rationale for mucosal vaccines and potential dual-use influenza/COVID-19 vaccines.
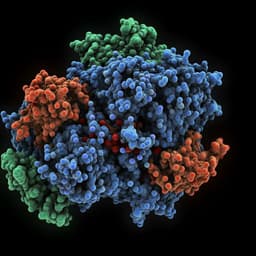
Vaccine design and generation: The LAIV backbone was derived from A/California/4/2009 (H1N1) (CA4) and A/Hong Kong/1968 (H3N2) (HK68) with NS1 deleted (DelNS1). The SARS-CoV-2 spike RBD sequence replaced NS1 in the NS segment. A tissue plasminogen activator (tPA) signal peptide was fused to the RBD N-terminus, and a 33-aa transmembrane plus cytoplasmic tail from human decay-accelerating factor (DAF) was fused to the C-terminus to ensure surface expression. To focus immunity on the ACE2-binding region, four N-glycosylation sites were introduced into RBD by mutations A372T, G413N, D428N, and P521N. Constructs were made for lineage A (WT), Beta (B.1.351), Delta (B.1.617.2), and Omicron BA.1 RBDs. Viruses were rescued by transfecting eight pH2000 plasmids (including the modified NS segment, HA/NA segments for CA4 or HK68, and remaining CA4 backbone segments) plus an NS1 expression plasmid into HEK293T cells, followed by passaging in embryonated chicken eggs and titration on MDCK cells. In vitro characterization: MDCK cells were infected to assess RBD expression with or without DAF by immunofluorescence. Western blots evaluated glycosylation-dependent expression profiles across cell lines (MDCK, BHK21, A549). Animal immunizations and challenges: Female BALB/c mice (6–8 weeks) were anesthetized and immunized intranasally with 2×10^6 pfu of CA4- or HK68-based DelNS1 vectors expressing RBD variants or empty vectors; boosts were given 4 weeks later with heterologous subtype vectors. In one comparison, mice received a single intramuscular dose of BNT162b2 (5 µg per mouse). Syrian hamsters received intranasal vaccines (5×10^6 pfu of DeltaN-DAF, BetaN-DAF, or OmicronN-DAF) or intramuscular BNT162b2 (1/6 clinical dose, 50 µg). Four weeks after boosts, animals were challenged: mice with mouse-adapted SARS-CoV-2 (Delta or Omicron BA.1 MA; 1×10^5 pfu); hamsters with Delta or Omicron BA.2 (1×10^6 pfu). Body weight, lung and nasal turbinate titers, and histopathology were assessed at defined dpi. Mouse-adapted virus generation: Gamma (P.1) and Omicron (BA.1) variants were serially passaged in BALB/c mice; lung homogenates were passaged to derive mouse-adapted strains. TCID50 assays determined titers; Sanger sequencing confirmed mutations. Sequences were deposited (GenBank OQ619913, OQ619914; GISAID EPI_ISL_12964908, EPI_ISL_12964907). Serology and neutralization: ELISAs quantified anti-RBD IgG and BALF IgA (Wantai kits). Pseudovirus neutralization used VSV-based pseudotypes with variant spikes and HIV-1 backbone, read by luciferase (IC50 via GraphPad). Live virus neutralization assessed CPE inhibition in TMPRSS2-expressing cells after 4 days; endpoint defined as 50% CPE inhibition. T-cell assays: Ten days post-boost, lung and spleen cells were stimulated with overlapping RBD peptide pools (lineage A) or influenza NP peptides. Intracellular cytokine staining measured IFN-γ and TNF-α in CD4+ and CD8+ T cells via flow cytometry. Tissue-resident memory markers (CD69, CD103) were assessed 5 weeks post-boost after intravascular staining. Ethics and biosafety: Animal protocols approved by HKU; SARS-CoV-2 work in BSL-3.
- Engineering RBD with a DAF membrane anchor in the DelNS1 vector markedly increased RBD surface expression in infected cells compared to RBD without DAF.
- Introducing four N-glycosylation sites to shield non-ACE2-competing epitopes enhanced immunogenicity, focusing responses to the ACE2-binding region.
- In mice, DelNS1-RBD4N-DAF (including Delta and Omicron BA.1 RBD versions) induced significantly higher anti-RBD IgG and stronger pseudovirus/live-virus neutralization than vectors lacking DAF; statistical analyses by one-way ANOVA with Dunnett’s test showed significant differences (p values often < 0.01 to < 0.0001).
- Intranasal vaccination elicited mucosal anti-RBD IgA in BAL fluid in mice for Delta and Omicron RBD LAIVs.
- In hamsters, intranasal Delta- and Beta-RBD4N-DAF induced higher RBD-specific antibodies and neutralization titers than controls; cross-neutralization varied by variant, with limited cross-neutralization against Omicron after Delta/Beta immunization, consistent with variant antigenic distances.
- DelNS1-RBD4N-DAF LAIVs induced robust T-cell responses: Delta RBD LAIV elicited both CD4+ and CD8+ responses in lungs and spleen; Omicron BA.1 RBD LAIV elicited strong CD4+ but weaker detectable CD8+ responses using lineage A peptide pools.
- Protection in mice: Intranasal DelNS1-RBDn-DAF conferred protection against mouse-adapted Omicron BA.1 challenge with no detectable lung virus at 2 and 4 dpi and preserved body weight.
- Protection in hamsters: Against Delta or Omicron BA.2 challenge, intranasal DeltaN-DAF or OmicronN-DAF reduced or prevented virus replication in lungs and nasal turbinates and mitigated weight loss. Three-dose BNT162b2 or two-dose BNT162b2 plus Omicron-DAF intranasal booster significantly reduced lung and nasal turbinate titers; near-sterilizing immunity in the LAIV groups was noted, with some groups showing ~100-fold reductions in lung titers relative to controls.
- Dual-function potential: DelNS1-RBDn-DAF LAIVs based on H1N1 or H3N2 backbones protected mice from lethal H1N1 or H3N2 influenza challenges, completely blocking lung viral replication, while retaining influenza-specific HA antibodies and NP-specific T-cell responses.
- Pre-existing influenza immunity did not abrogate SARS-CoV-2 RBD immunogenicity; mice previously infected with matched influenza strains still developed robust SARS-CoV-2-specific binding and neutralizing antibodies and were fully protected against Omicron BA.1 MA challenge.
The study addresses the key challenge of preventing SARS-CoV-2 infection at the site of entry by inducing strong mucosal immunity via an intranasal LAIV platform. Engineering the RBD to be displayed on infected cell membranes and focusing responses on the ACE2-binding epitopes enhanced immunogenicity, resulting in high systemic neutralizing antibodies, mucosal IgA, and robust T-cell responses. Functionally, LAIV immunization prevented or markedly reduced replication of highly transmissible variants (Delta, Omicron BA.2) in both upper and lower respiratory tissues in animal models, a level of protection not consistently achieved by intramuscular mRNA vaccination alone. These findings suggest that intranasal LAIVs could complement or boost existing systemic vaccine strategies to limit transmission. The platform’s ability to concurrently protect against influenza underscores its potential as a practical dual-use annual vaccine, aligning with the anticipated co-circulation of SARS-CoV-2 and influenza.
An NS1-deleted influenza virus vector expressing a membrane-anchored, glycan-engineered SARS-CoV-2 RBD (DelNS1-RBD4N-DAF) elicits strong systemic and mucosal immunity, robust T-cell responses, and provides near-sterilizing protection against SARS-CoV-2 variants in mice and hamsters. It also confers protection against influenza, supporting development as a dual-function intranasal vaccine for annual use. Future work should include clinical evaluation to confirm safety, mucosal immunogenicity, and effectiveness in preventing infection and transmission in humans, optimization against evolving variants (e.g., updated RBDs), and assessment of durability and booster strategies, including heterologous combinations with systemic vaccines.
- Findings are from preclinical mouse and hamster models; human efficacy and transmission impact remain to be established.
- T-cell analyses used peptide pools from the parental (lineage A) strain, potentially underestimating CD8+ responses to Omicron RBD due to sequence divergence; variant-specific peptide pools are needed.
- Cross-neutralization breadth varied by immunogen; Omicron-focused responses showed strain specificity, consistent with antigenic drift; breadth strategies may be needed for emerging variants.
- Prior clinical trials with earlier DelNS1-RBD versions could not fully quantify airway-specific immune responses, underscoring a need for direct mucosal immunogenicity measurements in future human studies.
- Some interspecies differences in response to mRNA vaccination were noted (e.g., differing IgG levels in mice vs hamsters), highlighting model-specific variability.
Related Publications
Explore these studies to deepen your understanding of the subject.