Medicine and Health
Ablation of the gut microbiota alleviates high-methionine diet-induced hyperhomocysteinemia and glucose intolerance in mice
W. Li, Y. Jia, et al.
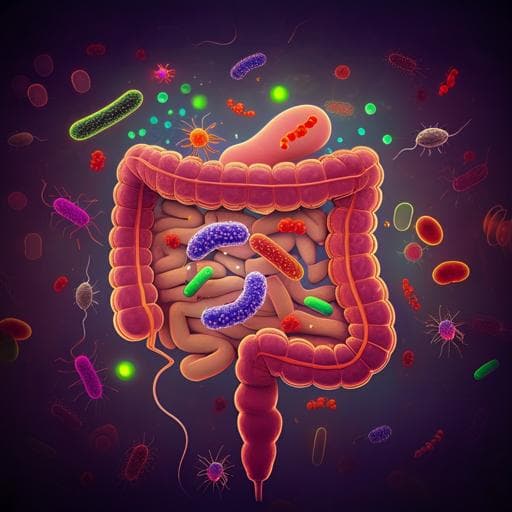
Hyperhomocysteinemia (HHcy), defined as plasma homocysteine >15 µmol/L, is a sulfur-containing amino acid byproduct of methionine metabolism and is an independent risk factor for cardiovascular diseases. HHcy has also been linked to glucose intolerance, insulin resistance, and hepatic steatosis in mice. Plasma Hcy levels are influenced by genetics, dietary methionine, B vitamins/folate status, and certain drugs. A high-methionine (HM) diet is a standard model to induce HHcy in animals. While the liver is a primary site for methionine/Hcy metabolism, isotope-tracer studies indicate the gastrointestinal tissue (GIT) metabolizes a substantial fraction of dietary methionine and is a net producer of Hcy. The gut microbiota, shaped strongly by diet, plays major roles in host metabolism, including amino acid metabolism (e.g., tryptophan). Whether gut microbes contribute to methionine/homocysteine metabolism and HHcy remains unclear. This study tests the hypothesis that gut microbiota contribute to HM diet-induced HHcy and glucose intolerance, and that their ablation mitigates these effects, potentially via reduced microbial Hcy production.
Prior work has established HHcy as a risk factor for atherosclerosis, hypertension, vascular calcification, aneurysm, and metabolic dysfunction. Dietary methionine acutely raises plasma Hcy in humans and is widely used to induce HHcy in animal models. The liver expresses key enzymes in methionine/Hcy metabolism (e.g., MAT, AHCY, BHMT, CBS) and is considered the central organ for these pathways. Nevertheless, tracer studies in piglets demonstrate that the GIT metabolizes about 20% of dietary methionine and is a net source of plasma Hcy, suggesting extrahepatic contributions. Diet robustly modulates gut microbial composition and function, and multiple microbial pathways regulate host amino acid metabolism (e.g., tryptophan). Correlative human data link certain gut taxa to plasma Hcy in Parkinson’s disease. However, causal evidence for gut microbiota involvement in HHcy, particularly under HM diet conditions, has been lacking.
Experimental design: Male C57BL/6J mice (8 weeks) were fed chow or a high-methionine (HM) diet (2% L-methionine; 20 g/kg) for 4 weeks. To deplete gut microbiota, a nonabsorbable broad-spectrum antibiotic (ABX) cocktail (neomycin 1 mg/mL, streptomycin 1 mg/mL, bacitracin 1 mg/mL) was provided in drinking water for 28 days. Mice were housed 3 per cage, 12-h light/dark cycle, ad libitum access to food/water. Food intake and body weight were monitored. Assessments: At study end, blood, liver, and intestinal epithelium were collected. Metabolic tests included glucose tolerance test (GTT; 12-h fast; 3 g/kg glucose i.p.) and insulin tolerance test (ITT; 4-h fast; 1 IU/kg insulin i.p.), with tail blood glucose measured at 0–120 min and area under curve (AUC) computed. Biochemical assays: Plasma homocysteine (Hcy) measured by enzymatic cycling on Hitachi 7600 analyzer. Plasma insulin by ELISA; triglyceride (TG) by GPO-PAP; total cholesterol (TC) by CHOD-PAP. Tissue LC-MS: Plasma methionine, intestinal epithelial methionine and homocysteine quantified by LC-MS (AB Sciex TripleTOF 5600). Sample prep used isotopic internal standards (D,L-homocysteine-d4; H3-L-methionine), DTT reduction, protein precipitation with acetonitrile/formic acid; analytes identified by retention time vs standards and quantified by external calibration. Liver molecular analyses: Hepatic mRNA expression of CBS, BHMT, MetRS, MAT1A, MAT2A, MTHFR by qRT-PCR (normalized to β-actin). Protein levels of CBS and BHMT by western blot (GAPDH loading control). Liver CBS enzyme activity measured with a kit monitoring H2S formation from cysteine+homocysteine (fluorescent readout). Liver S-adenosylmethionine (SAM) and S-adenosyl-L-homocysteine (SAH) by ELISA. Intestinal gene expression: mRNA levels of MetRS, MAT2A, BHMT, and SLC1A5 in intestinal epithelium by qRT-PCR. Histology: Colonic morphology assessed; noted changes with ABX under HM diet. Microbiome: Metagenomic shotgun sequencing of fecal DNA (NEBNext library prep; Illumina platform). Reads filtered and host-depleted (Bowtie2), assembled (SOAPdenovo/MEGAHIT), annotated taxonomically (DIAMOND vs NR, LCA with MEGAN) and functionally (KEGG). Diversity metrics (ACE, Chao1, Shannon), Bray–Curtis PCoA, ANOSIM, Metastats and LEfSe for differential taxa; KEGG pathway analysis for functional shifts. Microbial culture and metabolite detection: Dubosiella newyorkensis (ATCC) cultured anaerobically in chopped meat carbohydrate broth (24 h, 37°C). Supernatant collected and analyzed by LC-MS for homocysteine; identification by retention time (~3.47 min) compared with D,L-homocysteine standards. Statistics: Data expressed as mean ± SEM. Shapiro–Wilk for normality. Group comparisons by unpaired two-tailed Student’s t-test or one-way ANOVA with Tukey’s post hoc for normal data; Mann–Whitney for non-normal. P<0.05 considered significant. Sample sizes generally n=6 per group; some assays n=12 for plasma/tissue amino acids.
- Gut microbiota ablation reduces HM diet-induced hyperhomocysteinemia: • HM diet elevated plasma Hcy vs chow: 23.04 vs 10.04 µM (P<0.0001). • ABX reduced plasma Hcy in HM-fed mice: 13.67 vs 23.04 µM (P<0.0001). • ABX also modestly lowered Hcy under chow (7.92 vs 10.04 µM; trend P=0.0566 reported contextually).
- Methionine levels: • Plasma methionine increased with HM vs chow: 364.7 vs 63.6 µM (P<0.0001); no difference HM vs HM+ABX. • Intestinal epithelial methionine increased with HM vs chow: 37.58 vs 23.64 µg/g (P<0.0001); no difference HM vs HM+ABX.
- Intestinal epithelial homocysteine: • Increased with HM vs chow: 1.664 vs 1.007 µg/g (P<0.0001). • Reduced by ABX under HM: 1.360 vs 1.664 µg/g (P=0.0014).
- Glucose metabolism: • HM caused glucose intolerance (increased GTT AUC; P=0.0326), without significant change in insulin sensitivity (ITT AUC P=0.5915). • ABX improved glucose tolerance under HM (P<0.0001) with no significant effects on plasma insulin, TG, or TC across groups.
- Hepatic homocysteine metabolism enzymes: • HM diet did not alter hepatic mRNA/protein levels of CBS, BHMT, MetRS, MAT1A, MAT2A, MTHFR. • ABX increased hepatic mRNA of CBS, BHMT, MAT1A, MAT2A vs chow, but CBS/BHMT protein unchanged. • CBS enzymatic activity increased with HM (P=0.0017) but was not altered by microbiota depletion (P=0.0701 between HM and HM+ABX). • Liver SAM increased with HM (300.6 vs 258.8 ng/g; P=0.0033) and decreased with ABX under HM (254.1 vs 300.6 ng/g; P=0.0012). SAH unchanged.
- Microbiome composition shifts under HM diet: • Beta-diversity differed (Bray–Curtis PCoA P=0.004); alpha-diversity unchanged (ACE, Chao1, Shannon). • Family-level: decreased Lachnospiraceae and Rikenellaceae; increased Prevotellaceae. • Increased Erysipelotrichaceae (P=0.0022), including Faecalibaculum (P=0.0022) and Dubosiella (P=0.0043); decreased Rikenellaceae (P=0.0411) and Alistipes (P=0.0411). • Species-level increases: Faecalibaculum rodentium and Dubosiella newyorkensis (both P≤0.0043).
- Functional (KEGG) shifts: • Cysteine and methionine metabolism pathway upregulated in HM (P=0.0371). • Two homocysteine biosynthesis-related KOs were increased (K01739, K14155; P=0.0235 and P=0.0260), implicating enzymes in de novo methionine biosynthesis (e.g., CGS and CCBL) contributing to microbial homocysteine production.
- Correlations and direct detection: • Plasma Hcy positively correlated with Faecalibaculum abundance (r=0.7684, P=0.0035) and Dubosiella abundance (r=0.6632, P=0.0187). • Faecalibaculum positively correlated with bacterial CCBL gene abundance (r=0.7972, P=0.0019); Dubosiella with CGS gene abundance (r=0.6713, P=0.0168). • LC-MS detected homocysteine in Dubosiella newyorkensis culture supernatant with retention time ~3.47 min, matching standards.
The study demonstrates a causal role for gut microbiota in HM diet-induced hyperhomocysteinemia and glucose intolerance. While the liver is central to methionine/homocysteine metabolism, the gastrointestinal tract emerges as a significant net producer of Hcy, and its resident microbiota contribute to circulating Hcy under HM conditions. Antibiotic-mediated microbiota ablation reduced plasma and intestinal epithelial Hcy without altering plasma methionine, indicating that microbes utilize methionine to produce Hcy that is then exported to the host. Hepatic expression and activity of core Hcy-handling enzymes were largely unaffected by microbiota depletion in HM-fed mice, suggesting the primary effect occurs within the gut ecosystem rather than through hepatic enzyme modulation. The HM diet reshaped the gut microbiota, enriching Erysipelotrichaceae members (Faecalibaculum, Dubosiella) that correlated with both plasma Hcy and bacterial genes (CGS, CCBL) implicated in homocysteine biosynthesis in the de novo methionine pathway. Direct LC-MS detection of Hcy in D. newyorkensis culture supports microbial Hcy production. Functionally, increased microbial cysteine/methionine metabolism aligns with elevated microbial Hcy production. Microbiota depletion improved glucose tolerance under HM, likely secondary to reduced plasma Hcy, consistent with prior links between HHcy and impaired glucose handling. These findings highlight the gut microbiota as a modifiable source of Hcy influencing systemic metabolic phenotypes.
Gut microbiota are necessary for the full development of HM diet-induced hyperhomocysteinemia and associated glucose intolerance in mice. An HM diet reshapes the microbiota, enriching taxa (Faecalibaculum, Dubosiella) and functional capacities (CGS/CCBL-related KOs) that likely drive microbial homocysteine production and secretion. Ablation of gut microbes reduces plasma and intestinal Hcy and improves glucose tolerance without major changes in hepatic Hcy metabolism, positioning the intestine-microbiota axis as a therapeutic target. Future work should include mechanistic studies using microbial genetic perturbation (e.g., CGS/CCBL mutants), gnotobiotic models to establish causality of specific taxa, and clinical investigations to determine whether similar microbial and functional shifts occur in patients with HHcy and whether microbiota-targeted interventions can lower plasma Hcy.
- Clinical translation is limited: no human cohort data were provided to confirm microbiota compositional/functional changes in HHcy patients.
- Mechanistic attribution to specific enzymes/taxa remains correlative; CGS/CCBL roles were inferred and require validation using bacterial mutants and colonization studies.
- Antibiotic treatment can have off-target effects on host physiology and gut barrier/mucus, as evidenced by colonic structural alterations in HM+ABX mice; these effects may confound interpretations.
- Sample sizes were modest (generally n=6 per group), potentially limiting detection of smaller effects.
- Only male mice were studied; sex-specific effects were not assessed.
- Duration was 4 weeks; longer-term effects and reversibility were not evaluated.
Related Publications
Explore these studies to deepen your understanding of the subject.