Medicine and Health
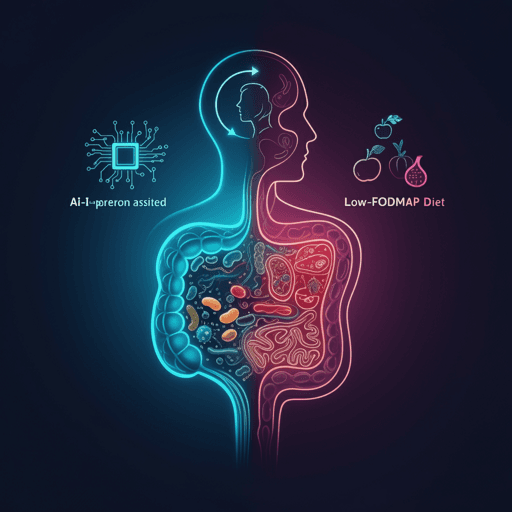
A Multicenter Randomized Controlled Trial of Microbiome-Based Artificial Intelligence-Assisted Personalized Diet vs Low-Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols Diet: A Novel Approach for the Management of Irritable Bowel Syndrome
V. Tunali, N. Ç. Arslan, et al.
A multicenter randomized trial found that an AI-assisted, microbiome-based personalized diet delivered notable symptom relief, improved quality of life, and measurable gut microbiome diversity shifts compared with a low-FODMAP diet over six weeks. This research was conducted by Varol Tunali, Naciye Çiğdem Arslan, Beyza Hilal Ermiş, Gözde Derviş Hakim, Aycan Gündoğdu, Mehmet Hora, and Özkan Ufuk Nalbantoğlu.
Related Publications
Explore these studies to deepen your understanding of the subject.