Medicine and Health
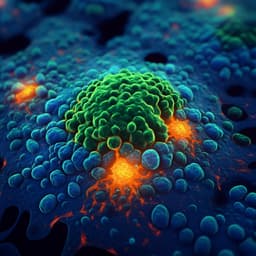
A bacteriocin-based antimicrobial formulation to effectively disrupt the cell viability of methicillin-resistant *Staphylococcus aureus* (MRSA) biofilms
C. Kranjec, K. V. Ovchinnikov, et al.
This study conducted by Christian Kranjec, Kirill V. Ovchinnikov, Torstein Grønseth, Kumar Ebineshan, Aparna Srikantam, and Dzung B. Diep reveals the promising synergistic antibacterial effects of garvicin KS and micrococcin P1 against *Staphylococcus aureus* biofilms, including MRSA strains. The combination not only inhibits cell viability but also revives MRSA susceptibility to penicillin G, pointing to bacteriocins as potential therapeutic agents against stubborn biofilm infections.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.