Medicine and Health
Two-year safety outcomes of iPS cell-derived mesenchymal stromal cells in acute steroid-resistant graft-versus-host disease
K. Kelly, A. J. C. Bloor, et al.
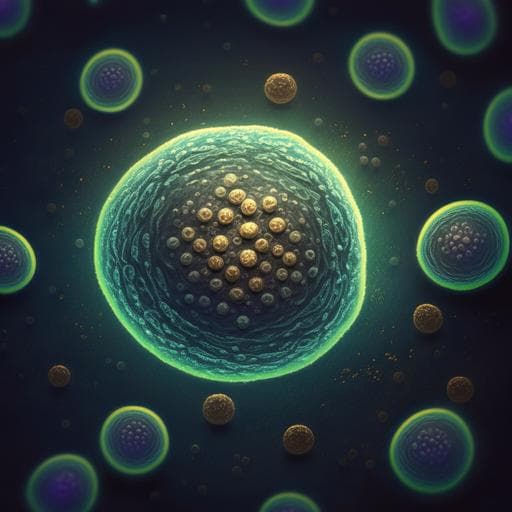
This clinical trial found that 60% of participants with steroid-resistant acute graft-versus-host disease survived after two years of treatment with iPS cell-derived mesenchymal stromal cells (CYP-001). Impressively, there were no serious adverse events or safety concerns reported, indicating that this innovative therapy is both safe and well-tolerated. This research was conducted by Kilian Kelly, Adrian J. C. Bloor, James E. Griffin, Rohini Radia, David T. Yeung, and John E. J. Rasko.
Related Publications
Explore these studies to deepen your understanding of the subject.