Medicine and Health
Therapeutic efficacy of a MMAE-based anti-DR5 drug conjugate Oba01 in preclinical models of pancreatic cancer
C. Zheng, D. Zhou, et al.
Pancreatic cancer (PC) is highly malignant, often asymptomatic until advanced stages, with ~60% of patients diagnosed at advanced disease and >90% unresectable; the 5-year survival rate is <9%. Chemotherapy is the current mainstay but with limited efficacy, underscoring an urgent need for new targets and therapies. Antibody-drug conjugates (ADCs) couple monoclonal antibodies to cytotoxic payloads via stable linkers, enabling antigen-directed delivery and intracellular toxin release; 14 ADCs have been approved across multiple cancers. Death receptor 5 (DR5; TRAIL-R2) is a TNFR superfamily receptor with low expression in normal tissues but high expression in many cancers, including pancreatic cancer, and can induce apoptotic/autophagic cell death. Despite clinical development of agonistic anti-DR5 antibodies, none has reached market. Previously, Zapadcine-1 (zaptuzumab-PY-VC-MMAD) showed potent antileukemic activity but a narrow safety window. An optimized ADC, Oba01 (zaptuzumab-PY-VC-MMAE), retained tumor specificity and lysosomal trafficking, exhibited potent antitumor activity in DR5-positive leukemia models, and demonstrated improved tolerability in rats and cynomolgus monkeys. The present study evaluates Oba01 in solid tumors, specifically pancreatic cancer, by quantifying DR5 expression in PC cell lines, patient tissues, and normal tissues; characterizing Oba01’s in vitro and in vivo antitumor activities and mechanisms; and assessing synergy with approved drugs. Results show robust antitumor activity in DR5-positive PC cell lines, CDX and PDX models, and synergy with gemcitabine, supporting clinical advancement of Oba01 for DR5-expressing PC.
Drugs and reagents: Oba01 (zaptuzumab-PY-VC-MMAE), its naked antibody (zaptuzumab), and MMAE were supplied by Yantai Mabplex International Bio-Pharmaceutical Co. Ltd.; gemcitabine from Selleck. A panel of primary and secondary antibodies was used for immunoblotting and IHC.
Cell lines: Human pancreatic cancer cell lines (Mia PaCa-2, PL45, PATU8988, JF305, PANC-1, Panc 10.05, Panc 05.04, BxPC-3), bladder cancer T24, and lung cancer Calu-1 were obtained from authenticated sources, STR-validated, mycoplasma-free, and cultured in RPMI-1640 with 10% FBS and antibiotics at 37°C, 5% CO2.
Gene expression analyses: Total RNA was isolated (TaKaRa). Reverse transcription used PrimeScript RT with gDNA eraser; qPCR used TB Green Premix Ex Taq II with primers for human DR5 and β-actin. Relative expression was calculated by the 2^-ΔΔCt method.
Protein analyses: Western blots were performed on SDS-lysed samples separated by SDS-PAGE, transferred to PVDF, probed with primary/secondary antibodies, and detected by ECL.
In vitro cytotoxicity: DR5-positive and -negative cells were treated with serial dilutions of Oba01 (triplicate) for 3 days in 10% heat-inactivated FBS media. Viability was measured by CellTiter-Glo and IC50 values calculated by nonlinear regression (GraphPad Prism). The coefficient of drug interaction (CDI) was used to assess drug interactions for combinations.
Internalization: Oba01-induced DR5 internalization was assessed as previously described, confirming receptor-mediated endocytosis in Mia PaCa-2 and PL45.
Apoptosis and cell cycle: Mia PaCa-2 and PL45 cells were treated with Oba01 (0–5 μg/mL for apoptosis; 0–25 μg/mL for cell cycle) for 48 h. Apoptosis was measured by Annexin V-FITC/PI flow cytometry. Cell cycle distribution was measured by DNA content flow cytometry.
Clonogenic assays: DR5 WT/KO Mia PaCa-2 and DR5 WT/OE T24 cells were seeded (3000 cells/well, 6-well plates), treated with Oba01 (0–5 μg/mL), incubated 1 week, fixed, crystal violet stained, and colonies (>50 cells) counted.
ADCC and CDC: For ADCC, Mia PaCa-2 and PL45 target cells were pretreated with Oba01 then co-incubated with IL-2-activated human PBMCs at E:T ratios (1:5, 1:20, 1:80) for 4 h; cytotoxicity assessed by LDH release (CytoTox 96). For CDC, human serum (20%) or heat-inactivated serum control was used with Oba01 for 4 h and lysis quantified by OD490.
Bystander killing: DR5-positive Mia PaCa-2-GFP or PL45-GFP and DR5-low/negative Calu-1-mCherry cells were cultured alone or mixed (2–2.5:1) and treated with Oba01 for 5 days; live cells quantified by flow cytometry to evaluate killing of DR5-negative neighbors.
Genetic modulation of DR5: Stable DR5 knockout in Mia PaCa-2 was generated via CRISPR/Cas9 using sgRNAs (gRNA1: 5′-ATAGTCCTGTCCATATTTGCAGG-3′; gRNA2: 5′-CGGCACTTCCGGCACATCTCAGG-3′). Monoclonal selection, sequencing, qPCR, and Western confirmed DR5 loss. DR5 overexpression in T24 (and Calu-1) was achieved via lentiviral transduction of DR5 cDNA with puromycin selection (2 μg/mL, ≥7 days), validated by qPCR/Western.
Animal studies: Female BALB/c nude mice (5–6 weeks) were used under IACUC-approved protocols. CDX models: subcutaneous injection of 5×10^6 PC cells (Mia PaCa-2, PL45, PATU8988, JF305). PDX models (PA1266, PA1198) established by subcutaneous implantation of 2–3 mm tumor fragments. When tumors reached 100–150 mm^3, mice were randomized (n=4–6/group). Treatments: Oba01 (5 or 10 mg/kg, IV, weekly ×3), zaptuzumab (10 mg/kg), MMAE (0.2 mg/kg; equimolar to 10 mg/kg Oba01), vehicle. Combination therapy: Oba01 (5 mg/kg) plus gemcitabine (25 or 40 mg/kg, IP) on indicated schedules. Tumor volumes measured twice weekly; T/C (%) = treated/control ×100; TGI (%) = (1−T/C)×100. Body weight monitored. Organs collected for histopathology.
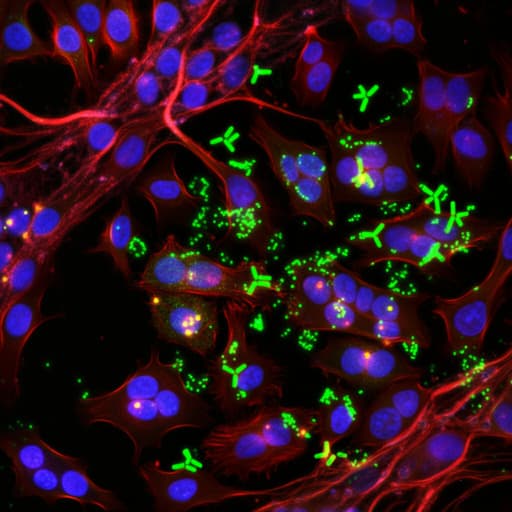
Histopathology/IHC: Patient PDAC TMAs (n=185) and normal pancreas were stained for DR5 (IHC) and H&E. Xenograft tumors underwent DR5 IHC and H&E. Imaging used TissueFAXS Plus.
Statistics: Data are mean ± SEM of ≥3 independent experiments. IC50 by nonlinear regression. Group comparisons by one-way ANOVA or Student’s t-test vs control. Significance: P<0.05 (* 0.01≤P<0.05; ** 0.001≤P<0.01; *** P<0.001).
-
DR5 expression in pancreatic cancer:
- Public dataset analysis (GEPIA) showed significantly higher DR5 mRNA in PC vs normal pancreas.
- IHC on 185 PDAC patient specimens: DR5 positive in 50.3% (93/185); moderate 9.2% (17/185), low 41.1% (76/185), negative 49.7% (92/185). DR5 undetectable in five normal pancreas tissues. DR5 predominantly membrane-localized with some cytoplasmic staining.
- Western blots: High DR5 in PC lines Mia PaCa-2, PL45, PATU8988, PANC-1, JF305, BxPC-3, Panc 05.04, Panc 10.05; low/none in Calu-1 and T24.
-
In vitro efficacy and DR5 dependence:
- Oba01 was highly cytotoxic to DR5-positive PC cells with IC50 range 4.79 ± 1.43 to 347.55 ± 150.54 nM; no inhibition in DR5-negative T24 and Calu-1.
- MMAE payload was broadly cytotoxic across all tested cells (IC50 0.06 ± 0.01 to 0.89 ± 0.24 nM), regardless of DR5.
- Oba01 induced DR5 internalization in Mia PaCa-2 and PL45.
- CRISPR/Cas9 DR5 knockout in Mia PaCa-2 and PL45 conferred resistance to Oba01; DR5 overexpression in T24/Calu-1 increased Oba01 sensitivity. Clonogenic assays corroborated DR5 dependence.
-
Mechanisms of action in vitro:
- Apoptosis: Dose-dependent increase in Annexin V+/PI+ cells in Mia PaCa-2 and PL45; increased PARP cleavage; decreased MCL-1, p-AKT, and p-mTOR.
- Cell cycle: G2/M-phase arrest with reduced G0/G1 in DR5-positive cells.
- Bystander effect: In mixed cultures, Oba01 killed DR5-negative Calu-1/mCherry when co-cultured with DR5-positive Mia PaCa-2-GFP or PL45-GFP, indicating diffusion of cytotoxic MMAE.
- ADCC: Oba01 mediated PBMC-dependent cytotoxicity in Mia PaCa-2 and PL45, enhanced with higher E:T ratios.
- CDC: With human serum, lysis increased to ~40.01 ± 0.55%–42.39 ± 3.88% (Mia PaCa-2) and ~31.02 ± 9.19%–34.16 ± 1.45% (PL45) vs serum alone ~26.29 ± 3.39%–27.54 ± 0.81% and 7.66 ± 5.47%–13.57 ± 1.73%, respectively; heat-inactivated serum showed minimal lysis (~0–9.64 ± 1.69%).
-
In vivo efficacy (CDX):
- Mia PaCa-2: Oba01 5 mg/kg achieved TGI 84.37%; 10 mg/kg yielded complete regressions (CR) in 5/5 mice by day 12. MMAE (0.2 mg/kg) and zaptuzumab (10 mg/kg) showed no tumor inhibition.
- PL45: Oba01 5 mg/kg TGI 51.13%; 10 mg/kg TGI 92.94%.
- Additional CDX models (PATU8988, JF305) confirmed robust efficacy (qualitative).
- Tolerability: No significant body weight loss; H&E showed no overt toxicity in heart, liver, spleen, lung, kidney.
- DR5 IHC positive in all CDX tumors, supporting DR5-dependent activity.
-
Combination with gemcitabine:
- In vitro across PC lines, Oba01 + gemcitabine showed synergy (CDI<1), enhanced apoptosis (increased cleaved PARP), downregulated p-AKT/p-mTOR, CDK4, cyclin D1/E1, consistent with reinforced G2/M arrest and apoptotic signaling.
- CDX combination: In Mia PaCa-2, combination superior to monotherapies; CR in 5/6 mice during days 22–71 (one relapse day 55 but overall improved control). In PL45, combination also significantly superior to single agents.
-
In vivo efficacy (PDX):
- PA1266: Oba01 dose-dependent tumor regression; TGI 93.33% (5 mg/kg) and 97.46% (10 mg/kg). Combination (Oba01 5 mg/kg + gemcitabine 40 mg/kg) exceeded either monotherapy but slightly less effective than Oba01 10 mg/kg.
- PA1198: Oba01 TGI 54.22% (5 mg/kg) and 76.69% (10 mg/kg). Combination (Oba01 5 mg/kg + gemcitabine 25 mg/kg) significantly outperformed monotherapies.
- DR5 IHC positive in all PDX tumors; combination well-tolerated with stable body weight and no organ toxicity on histology.
Overall, Oba01 shows potent, DR5-dependent antitumor activity via multiple mechanisms and demonstrates strong synergy with gemcitabine in vitro and in vivo.
This study addresses whether targeting DR5 with an MMAE-based ADC (Oba01) can provide effective therapy for pancreatic cancer and whether efficacy can be enhanced by combination with standard agents. The data demonstrate that DR5 is frequently and predominantly membrane-expressed in PDAC cells and xenografts, enabling efficient Oba01 binding, internalization, and lysosomal release of MMAE. Oba01 induces G2/M arrest, apoptosis, and exerts a bystander effect, while its antibody component adds ADCC and CDC, providing multi-pronged cytotoxicity. Genetic modulation experiments establish DR5 as essential for Oba01 sensitivity, indicating potential resistance through DR5 loss and suggesting DR5 upregulation as a sensitizing strategy. In vivo, Oba01 monotherapy achieves deep and durable tumor regressions in multiple CDX and PDX models with favorable tolerability. Combination with gemcitabine yields synergistic antitumor effects, mechanistically linked to enhanced apoptosis (PARP-dependent), cell-cycle suppression (downregulation of CDK4, cyclin D1/E1), and inhibition of PI3K/AKT/mTOR signaling, consistent with complementary mechanisms (microtubule disruption by MMAE and DNA damage/ER stress by gemcitabine). Although overall IHC DR5 intensity did not strictly correlate with efficacy, membrane localization appears critical, highlighting the need for biomarker strategies focused on cell-surface DR5. These findings support advancing Oba01, alone and with gemcitabine, into clinical evaluation for DR5-expressing pancreatic cancer.
Oba01, a DR5-targeting MMAE-based ADC, exhibits strong preclinical antitumor activity against pancreatic cancer via apoptosis induction, G2/M cell-cycle arrest, bystander killing, and immune effector functions (ADCC/CDC). It achieves significant tumor regression and complete responses in CDX and PDX models with good tolerability. Combination with gemcitabine provides synergistic efficacy, mechanistically reinforcing apoptotic and antiproliferative signaling and suppressing PI3K/AKT/mTOR. These results position Oba01 as a promising biotherapeutic candidate for DR5-expressing pancreatic cancer and support clinical trials of Oba01 as monotherapy and in combination with gemcitabine. Future research should refine patient selection biomarkers (emphasizing membrane DR5), define minimal DR5 thresholds for response, and explore combinations with targeted agents or immunotherapies across solid tumors.
- Biomarker uncertainty: DR5 total IHC intensity did not consistently predict response; membrane localization may be more relevant but is challenging to quantify in clinical samples.
- Resistance mechanisms: Loss or downregulation of DR5 confers resistance; strategies to prevent or overcome this require investigation.
- Translational gap: Efficacy and safety are preclinical; human pharmacokinetics, safety, and efficacy remain to be established.
- Mechanistic scope: While PI3K/AKT/mTOR suppression and apoptosis markers were studied, additional pathways contributing to synergy with gemcitabine and bystander effects warrant further exploration.
- Limited breadth of in vivo models: Although multiple CDX and two PDX models were tested, broader genetic diversity and orthotopic/metastatic models could further validate efficacy and safety.
Related Publications
Explore these studies to deepen your understanding of the subject.