Medicine and Health
The microbiota–gut–brain axis in mental and neurodegenerative disorders: opportunities for prevention and intervention
L. K. Yassin, J. Skrabulyte-barbulescu, et al.
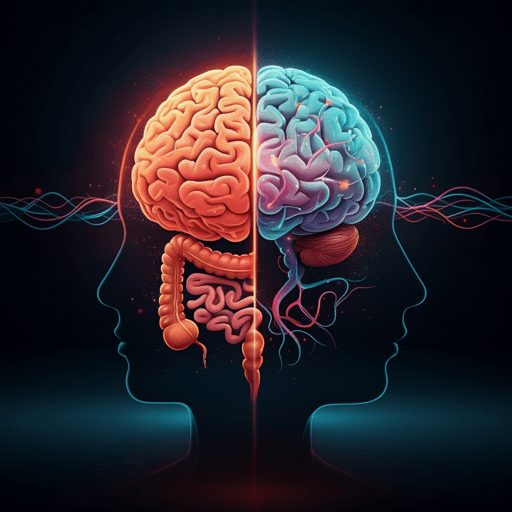
The review examines how the microbiota–gut–brain axis (MGBA) influences brain development, function, and disease across the lifespan. It frames a central question: how do gut microbial alterations contribute to neurodevelopmental, neurodegenerative, and neuropsychiatric disorders, and can modulating the gut microbiome prevent or mitigate CNS pathology? The introduction outlines bidirectional gut–brain communication via neural (vagus nerve, ENS), immune (cytokines, T cells), endocrine (HPA axis), and metabolic pathways (microbial metabolites such as SCFAs, bile acids). Germ-free and antibiotic-exposed animal models demonstrate causal roles for microbiota in neurodevelopmental abnormalities, stress responsivity, and behavior. Early-life microbial perturbations and external factors (e.g., radiation, xenobiotics) disrupt gut-brain homeostasis. The authors highlight widespread links between dysbiosis and diverse conditions (AD, PD, ALS, MS; MDD, BD, anxiety, PTSD; CFS; stroke) and set a translational objective: synthesize mechanistic evidence and evaluate preventative and interventional strategies (diet, psychobiotics, SCFAs, FMT) to restore gut–brain communication.
This narrative review synthesizes animal and human evidence on MGBA involvement in major neurodegenerative (AD, PD, ALS, MS, stroke/PSCI) and neuropsychiatric disorders (MDD, BD, anxiety, PTSD, CFS). It collates consistent dysbiosis patterns (reduced diversity, depletion of SCFA producers such as Faecalibacterium and Prevotella, enrichment of Proteobacteria and other pathobionts), mechanistic pathways (neuroinflammation, BBB dysfunction, microglial activation, neurotransmitter imbalances), and disease-specific microbial signatures. For AD, the review summarizes amyloid/tau biology, stress and HPA axis dysregulation, bile acids signaling (FXR, TGR5, S1PR2), and multiple human/animal studies linking altered microbiota and metabolites with pathology; tables compile probiotic and FMT data. PD sections cover prodromal GI symptoms, vagus nerve involvement, frequent taxa shifts (↓Prevotella, ↑Akkermansia/Verrucomicrobiaceae), medication/device effects (L-DOPA, DBS, LCIG) on microbiota, and trials of probiotics/prebiotics/FMT. ALS evidence highlights decreased beneficial taxa, increased pro-inflammatory species, systemic inflammation, and early reports of FMT. MS literature discusses immune regulation (Th17/Treg), increased Akkermansia and Methanobrevibacter with reduced SCFA producers, and pilot probiotic/FMT data; tables summarize taxa changes. Mood/anxiety/PTSD/CFS sections integrate microbiome signatures, metabolite changes (SCFAs, kynurenine pathway), and psychobiotic/prebiotic/dietary trials. The review also covers radiation-induced MGBA disruption and xenobiotics (microplastics, glyphosate, antibiotics) as modulators of gut–brain signaling. Across topics, confounders (diet, geography, medications, sequencing approaches) and heterogeneity are acknowledged.
This is a narrative review that integrates and discusses findings from preclinical (germ-free, antibiotic-treated, stress models, toxin exposure, irradiation) and clinical studies (case reports, cohort studies, randomized controlled trials) across disorders relevant to the MGBA. Evidence includes taxonomic and functional microbiome profiling, metabolomics, immune biomarkers, and behavioral/cognitive outcomes, alongside schematic figures and summary tables (e.g., AD probiotic/FMT trials; PD device-assisted therapy effects; MS taxa alterations). No formal systematic search protocol or meta-analytic methods are described; instead, the authors compile recent advances and highlight mechanistic and translational themes.
- Cross-condition MGBA patterns: Dysbiosis characterized by reduced microbial diversity, depletion of SCFA-producing genera (e.g., Faecalibacterium, Prevotella, Coprococcus), and enrichment of pro-inflammatory/pathobiont taxa (e.g., Proteobacteria, Enterobacteriaceae) is common across AD, PD, ALS, MS, stroke, MDD, BD, anxiety, PTSD, and CFS. These changes correlate with neuroinflammation, BBB dysfunction, microglial and astrocytic activation, and neurotransmitter imbalances (serotonin, dopamine, GABA).
- Alzheimer’s disease (AD): Altered gut microbiota and bile acids profiles associate with CSF amyloid/tau biomarkers. Bile acids modulate CNS and gut immunity via FXR, TGR5, S1PR2; animal data show neuroprotection with TGR5 activation. Probiotics and prebiotics (e.g., Lactobacillus plantarum; Bifidobacterium breve) improve cognition and reduce amyloid/tau and neuroinflammation in AD models; early human case reports of FMT show improvements in cognition, mood, and microbiota diversity. Mediterranean diet (MeDi) and high-fiber intake associate with delayed cognitive decline and favorable microbiota/SCFA changes.
- Parkinson’s disease (PD): Consistent taxa shifts include ↓Prevotellaceae/Prevotella/P. copri and ↑Akkermansia/Verrucomicrobiaceae; constipation affects ~60% of PD and relates to dysbiosis (e.g., ↑Akkermansia). Microbiota influence L-DOPA pharmacodynamics (bacterial decarboxylation), and device-assisted therapies (DBS, LCIG) alter gut community structure. Probiotics improved GI symptoms and some non-motor/motor measures in trials; prebiotics (resistant starch) increased butyrate and improved non-motor symptoms; FMT case reports and animal studies suggest motor/cognitive benefits, but routine clinical use is not yet supported.
- ALS: Decreased beneficial taxa (e.g., Faecalibacterium) and increased potentially harmful species (e.g., E. coli) reported; systemic inflammation correlates with dysbiosis. Preliminary FMT reports and a phase II trial suggest possible stabilization/slowing of progression in subsets; mechanistic links include SCFA deficits, endotoxemia, BBB compromise, and microglial activation. Nutritional interventions (high-calorie/high-fat; timely PEG) are clinically relevant.
- MS: Increased Akkermansia/Methanobrevibacter and reduced SCFA producers associated with disease activity and Th17/Treg imbalance; small trials show probiotics can modulate immune markers and may improve clinical symptoms; case reports and pilot studies of FMT suggest improved gait and sustained increases in SCFAs/BDNF, but evidence remains preliminary.
- Stroke/PSCI: Stroke induces gut dysbiosis that worsens neuroinflammation and permeability; gut-derived immune cells and microbes can translocate (gut–brain, gut–lung axes). Modulating the microbiome (antibiotics, prebiotics, SCFA enhancement, diet) impacts infarct size, immune responses, and recovery in animal models; MeDi associates with increased diversity and SCFAs and reduced inflammation.
- Mood and anxiety disorders: MDD linked to reduced anti-inflammatory taxa (Faecalibacterium, Coprococcus) and altered Firmicutes/Bacteroidetes ratios; psychobiotics and synbiotics show improvements in mood and stress markers in RCTs. Anxiety disorders exhibit consistent beta-diversity shifts and depletion of butyrate producers; psychobiotics/probiotics and tryptophan-rich diets improve anxiety-like behaviors and restore MGBA signaling in preclinical models and small trials.
- Bipolar disorder (BD): Reduced α-diversity and altered taxa (↑Actinobacteria/Coriobacteria; ↓Ruminococcaceae/Faecalibacterium) correlate with inflammation (IL-6), metabolic disturbances, and symptom severity; adjunct probiotics reduced rehospitalizations after acute mania in one RCT, while another showed no symptom change, indicating strain- and context-specific effects.
- PTSD: Depletion of SCFA producers (Lachnospiraceae, Ruminococcaceae) with enrichment of pathobionts (Enterococcus, Escherichia/Shigella, Collinsella, Veillonella) correlates with symptom severity; FMT from PTSD patients induces anxiety-like behaviors in germ-free mice; MeDi reduces CRP and symptom severity, and prebiotics exhibit sex-specific benefits.
- CFS/ME: Consistent reductions in butyrate producers and enrichment of Enterobacteriaceae; dysbiosis linked to fatigue, cognitive dysfunction, and immune activation; probiotics/synbiotics and MeDi-type diets show potential symptomatic benefits; multi-omics support microbial-metabolite involvement.
- Radiation and xenobiotics: Pelvic/cranial irradiation disrupts gut microbiota (↓Firmicutes/Bacteroidetes; ↑Proteobacteria), increases LPS-driven inflammation, and contributes to neuroinflammation and cognitive impairment; microbial metabolites (butyrate, indole-3-propionic acid) confer neuroprotection in models. Microplastics, glyphosate, and antibiotics perturb MGBA, producing anxiety/depression-like behaviors via dysbiosis, barrier disruption, immune activation, and neurotransmitter changes; interventions (polyphenols, bile acids, probiotics/prebiotics) can reverse some effects in models. Overall, microbiome-targeted strategies (dietary patterns, fiber/SCFAs, probiotics, prebiotics, FMT) show promise across conditions but require rigorous clinical validation, standardized protocols, and mechanistic dissection.
The synthesis supports a central role for the MGBA in the pathophysiology of neurodegenerative and neuropsychiatric disorders. Shared mechanisms—dysbiosis-driven neuroinflammation, BBB compromise, microglial/astrocytic activation, HPA axis dysregulation, and altered neurotransmission—explain convergent features across heterogeneous diseases. The gut microbiota emerges as a modifiable determinant of brain health: dietary patterns (e.g., Mediterranean diet), fiber and SCFA augmentation, targeted psychobiotics, and FMT can restore gut–brain communication, ameliorate immune dysregulation, and improve cognitive/emotional outcomes in preclinical studies and early human trials. These findings address the review’s translational question by mapping mechanistic pathways to actionable interventions. However, disorder-specific microbial signatures, treatment effects (e.g., PD medications, device therapies), and host factors (sex, genetics, geography, diet) necessitate precision approaches. The discussion emphasizes the need to disentangle causality, refine strain/consortia selection, and integrate microbiome profiles with clinical phenotypes to optimize preventive and adjunctive therapies for healthier brain aging and improved disease outcomes.
This review consolidates evidence that the microbiota–gut–brain axis is a key, modifiable contributor to neurodevelopmental, neurodegenerative, and neuropsychiatric disorders. Across conditions, gut dysbiosis is both cause and consequence of CNS pathology, forming self-reinforcing loops involving inflammation, immune activation, and barrier dysfunction. Multiple microbiota-targeted interventions—probiotics, prebiotics, SCFA supplementation, dietary modification (e.g., Mediterranean and high-fiber diets), fecal microbiota transplantation, and emerging live biotherapeutic products (LBPs)—show promise for symptom alleviation and potential disease-modifying effects. Future research should: (1) perform mechanistic, causal studies to link specific microbes/metabolites to neurological outcomes; (2) conduct longitudinal, standardized clinical trials to establish efficacy, durability, and safety of microbiota-based therapies across diverse patient populations; (3) develop personalized strategies integrating microbiome, genetic, metabolic, and lifestyle data; and (4) rigorously characterize and standardize LBPs to transition microbiome-targeted approaches from adjuncts to medical-grade therapies capable of preventing or slowing disease progression.
- Evidence base is heterogeneous across studies with variable designs, small sample sizes, and differing sequencing/analytical pipelines, limiting comparability and reproducibility.
- Causality remains insufficiently established in many human contexts; associations may be confounded by diet, geography, medications (e.g., PD therapies), comorbidities, and environmental exposures.
- Intervention studies (probiotics, prebiotics, FMT, diet) often use diverse strains, doses, and durations, with preliminary or mixed outcomes; long-term safety and durability data are limited, especially for FMT.
- Device-assisted therapies and drugs can independently reshape microbiota, complicating attribution of disease-specific signatures.
- Sex differences and developmental timing effects are underexplored; many preclinical studies rely on male rodents.
- Standardized protocols for microbiota modulation and integrated multi-omics/biomarker frameworks are lacking, hindering clinical translation.
Related Publications
Explore these studies to deepen your understanding of the subject.







