Medicine and Health
Single-cell transcriptomics reveals aberrant skin-resident cell populations and identifies fibroblasts as a determinant in rosacea
M. Chen, L. Yang, et al.
Rosacea is a chronic inflammatory skin disorder primarily affecting the central face, with prevalence estimates ranging from under 1% to 22% worldwide. Clinically it manifests with facial erythema, telangiectasia, edema, papules, pustules, and recurrent flushing, and is categorized into erythematotelangiectatic (ETR), papulopustular (PPR), phymatous (PhR), and ocular subtypes, with overlapping features. Proposed pathogenesis includes impaired skin barrier function, dysregulated inflammatory responses with perivascular or pilosebaceous infiltration, hyperactive neurovascular reactivity and vasodilation, glandular hyperplasia, and fibrotic changes. Prior mechanistic insights have relied on histomorphology, bulk gene expression, and immunohistochemistry, in part because available laboratory models incompletely recapitulate rosacea. Single-cell RNA sequencing (scRNA-seq) enables delineation of cellular composition, rare subpopulations, transcriptional states, and intercellular communication at high resolution, yet had not been applied to rosacea. This study aims to define the skin-resident cellular landscape of rosacea at single-cell resolution across subtypes and to identify key cellular determinants and pathways driving inflammation, barrier dysfunction, and vascular abnormalities.
The study situates rosacea within a framework of barrier dysfunction, immune dysregulation, and neurovascular abnormalities described in prior literature. Earlier work documented diminished barrier integrity with reduced claudin expression, increased serine protease activity and cathelicidin driving inflammation, and neurovascular reactivity contributing to clinical features. Conventional analyses lacked cell-type resolution. scRNA-seq has characterized cellular heterogeneity in other skin diseases (e.g., psoriasis, atopic dermatitis), identifying fibroblast and immune subsets relevant to inflammation, but no single-cell atlas existed for rosacea before this work. The authors also discuss reports implicating interferon signaling in skin disease; while type I IFNs can rise in acute rosacea flares linked to dysbiotic commensals, the current work emphasizes type II IFN (IFNγ) from T cells as a driver of keratinocyte barrier gene suppression in stable disease contexts.
Human cohort: Skin biopsies were obtained from 9 female rosacea patients (3 ETR, 3 PPR, 3 PhR), sampling both lesional and non-lesional facial skin, and from 3 female healthy individuals’ facial skin. Ethical approval and informed consent were secured. Tissue processing separated epidermis and dermis, enzymatically dissociated each, pooled cells, removed dead cells, and generated single-cell suspensions within 3 hours of collection. scRNA-seq: Using 10x Genomics Chromium Single Cell 3' v3.1 kits, libraries were sequenced on Illumina NovaSeq 6000. Raw reads were aligned to hg38 with Cell Ranger v6.0.2. Quality control excluded cells with <200 or >6000 detected genes and >20% mitochondrial reads. A total of 131,243 cells passed QC. Normalization and scaling used Seurat v4.3.0 SCTransform. Clustering employed Louvain algorithm on first 20 PCs at resolution 0.6; UMAP was used for visualization. Marker genes were identified by Wilcoxon rank-sum test with thresholds avg_logFC ≥ 0.25 and adjusted p ≤ 0.05. Major cell types were annotated by canonical markers and subclustering performed per lineage (keratinocytes, fibroblasts, Schwann cells, vascular mural cells, endothelial cells, T cells, macrophages/DCs) using the first 20 PCs and appropriate resolutions. Differential expression and enrichment: DEGs between conditions used Seurat FindMarkers (min.pct > 0.25, logFC threshold 0.25, adjusted p < 0.05). Gene set enrichment analyses (GO/KEGG) were performed with clusterProfiler v4.5.1.902 and visualized with ggplot2; two-sided permutation tests were used without multiple comparison adjustment for GSEA visualizations. Cell-cell communication: CellChat v1.1.3 inferred intercellular ligand–receptor networks, considering cell types with >10 cells, using trimean for average expression and retaining interactions with p < 0.05. Incoming/outgoing interaction strengths and pathway contributions were compared across healthy, non-lesional, and lesional conditions. Validation and functional experiments: Immunohistochemistry and immunofluorescence on human and mouse skin assessed markers including KRT14, CD74, IRF1, p-STAT1, claudins (e.g., CLDN4), DCN, complement C3, MBP, CD69, CD103, α-SMA, p-MLC2, CCL19, CD4, CCR7, PTGDS, Vimentin, PTGDR, CD31. TEWL was measured with a Tewameter TM 300. PGD2 levels were quantified by ELISA. Mouse models: LL37-induced rosacea-like dermatitis was generated by intradermal injections (40 µl, 320 µM) twice daily for 2 days. IFNγ function was tested by daily subcutaneous neutralizing antibody injections around LL37 dosing. Fibroblast depletion used Col1a2-CreER crossed with iDTR mice (Col1a2DTR): tamoxifen IP for 5 days, followed by intradermal diphtheria toxin for 3 days, then LL37 challenge. PTGDS function was examined by intradermal siRNA knockdown (Ptgds or scrambled control). Outcomes included clinical scoring of redness area and severity, histology (H&E), immune cell infiltration counts, RT-qPCR of inflammatory and barrier genes, vascular assessments (CD31 perimeter, p-MLC2). Statistical analyses used Student’s t-tests, one-way ANOVA with Tukey’s post hoc, two-way ANOVA with Holm–Sidak where applicable, and Mann–Whitney U for non-normal data. Experiments were replicated at least three times with 5–6 mice per group, random allocation, and sex-matched groups (results shown for females).
- Cell atlas: 131,243 single cells from healthy skin and rosacea patients (lesional and non-lesional; ETR, PPR, PhR) revealed 11 major cell types and 28 clusters. Significant compositional shifts occurred in rosacea.
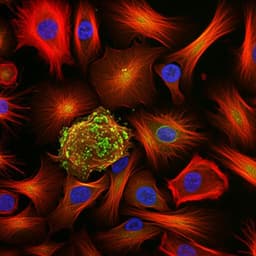
- Immune infiltration: T cells were the dominant infiltrates and increased in lesional skin of all subtypes and even in non-lesional PPR and PhR. Reported T cell proportions: HS 1.398%, ETR_N 1.586%, ETR_L 5.767%, PPR_N 7.536%, PPR_L 36.241%, PhR_N 3.97%, PhR_L 8.682%. Macrophages/DCs increased notably in PPR lesions (HS 1.058% vs PPR_L 2.03%) and slightly in ETR/PhR; mast cells were unchanged; B cells markedly increased in PPR lesions (HS 0.023% vs PPR_L 1.749%). Endothelial cells increased in PPR and slightly in PhR (HS 0.387% vs PPR_L 3.327%, PhR_L 4.202%). Due to immune infiltration, keratinocytes decreased across lesions (HS 93.82% vs PPR_L 43.90%).
- Keratinocytes: Identified a disease-enriched CD74+ keratinocyte subpopulation expanded in lesional skin across subtypes (most in PPR). GSEA showed upregulated interferon-related pathways and downregulated skin barrier pathways (tight junction, adherens junction, cell adhesion molecules), including reduced claudins (CLDNs). IFNγ (from T cells) was specifically upregulated; type I IFNs were not detected in these datasets. Immunostaining confirmed IRF1 and p-STAT1 activation.
- IFNγ function: In LL37-induced mice, IFNγ neutralization dampened IFNγ signaling, alleviated rosacea-like phenotypes, reduced dermal infiltration, lowered inflammatory gene expression (e.g., Il1b, Il6, Tnfa), reduced expansion of CD74+ keratinocytes, restored barrier gene expression (CLDNs, TJPs), and improved TEWL.
- Fibroblasts: Subclustering defined five fibroblast subpopulations (C3+, IGFBP3+, SFRP2+, ASPN+, DSG1+). C3+ fibroblasts were unique to PPR lesions and expanded (validated by C3/DCN co-staining). GSEA indicated pro-inflammatory programs (chemokine, cytokine–receptor, TNF, NF-κB). C3+ fibroblasts highly expressed chemokines CCL19, CXCL1, CXCL2, CXCL12; these chemokines were fibroblast-specific among all skin cell types. IFNγ neutralization reduced CCL19 in fibroblasts in mice.
- Schwann cells: Two subclusters identified; CD74+ Schwann cells expanded in PPR lesions (human), with upregulated inflammatory pathways (IL-17, TLR, antigen presentation), supporting neurogenic inflammation involvement.
- T cell states: Seven T-cell subclusters showed increased Th1 (IFNG, TBX21) and Th17 (IL17A, RORC) in PPR and to lesser degrees in ETR/PhR; Th2 slightly increased; Tregs increased in PPR/PhR. Resident memory T cells (TRM; ITGAE/CD103+, CD69+) were mildly expanded and confirmed by IHC.
- Macrophages/DCs: Macrophages increased (especially in PPR) and upregulated chemokines involved in T cell recruitment/activation (CCL5, CXCL9/10/11/12). GSEA highlighted complement/coagulation, antigen presentation, TLR signaling. CXCL10+ macrophages rose in mice and were reduced by IFNγ neutralization.
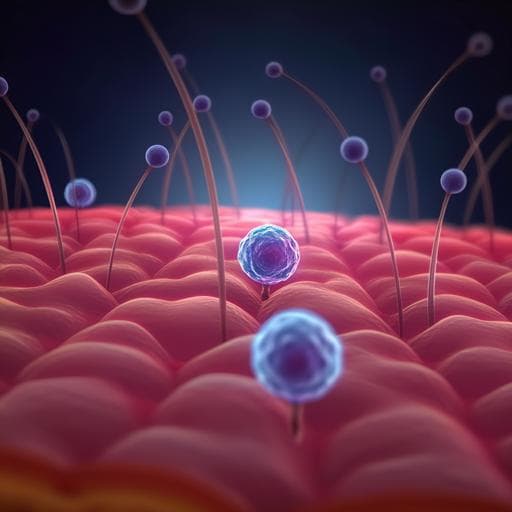
- Vascular cells: vSMCs and pericyte subcluster proportions were similar across conditions, but both exhibited upregulated inflammatory pathways (e.g., IL-17, NF-κB). Functionally, p-MLC2+ vMCs were dramatically decreased in lesions across subtypes, indicating impaired contractility; total MLC2 unchanged. Endothelial subcluster 1 increased in lesions with enriched type I IFN signaling.
- Cell–cell communication: CellChat showed increased interaction numbers/strengths in lesions (especially PPR). Fibroblasts were predominant senders of outgoing signals; T cells, B cells, macrophages, endothelial cells, vMCs, and keratinocytes were key recipients. Fibroblasts overrepresented in pro-inflammatory (chemokine, cytokine–receptor) and vasodilative (relaxin) categories; expressed high CCL19 engaging CCR7+ T cells, and specifically upregulated PTGDS.
- PTGDS/PGD2 axis: PTGDS was fibroblast-specific and increased in rosacea (notably ETR/PPR). PGD2 levels were significantly elevated in lesions; PTGDR (PGD2 receptor) was highly expressed in vMCs, supporting fibroblast-driven vasodilation.
- Functional causality: Fibroblast ablation in Col1a2DTR mice prevented development of LL37-induced rosacea-like dermatitis and reduced inflammation. Ptgds siRNA knockdown reduced PTGDS and PGD2, improved clinical features, decreased dermal infiltrates and inflammatory factors, reduced CCL19+ fibroblasts and CCR7+ T cells, and ameliorated vascular dilation (reduced CD31 vessel perimeter; restored p-MLC2).
The study addresses the central question of which skin-resident cell types and pathways drive rosacea pathogenesis. Single-cell profiling reveals that IFNγ from T cells drives a distinct CD74+ keratinocyte state with hyperactive interferon signaling and barrier gene suppression, offering a mechanistic link to the compromised epidermal barrier observed in rosacea and its contribution to inflammation. Immune remodeling features Th1/Th17 polarization, increased macrophages with T cell–recruiting chemokines, and expansion of TRM cells, potentially explaining chronicity and recurrence. Neurogenic components are supported by identification of pro-inflammatory Schwann cell subsets in lesions. Vascular dysfunction is linked to decreased p-MLC2 in vascular mural cells, indicating post-transcriptional impairment of contractility, and increased endothelial subsets with inflammatory signatures. Integrative cell–cell communication analyses position fibroblasts as central organizers: they are the dominant sources of inflammatory chemokines (e.g., CCL19 recruiting CCR7+ T cells) and vasodilatory mediators (PTGDS producing PGD2 acting on PTGDR-expressing vMCs). Functional experiments in mice corroborate causality: IFNγ blockade restores barrier function and reduces inflammation; fibroblast ablation prevents disease; Ptgds knockdown alleviates inflammation and abnormal vasodilation. Together, these findings elevate fibroblasts from bystanders to key determinants orchestrating immune and vascular networks in rosacea and highlight actionable axes (IFNγ–keratinocyte barrier, fibroblast CCL19–CCR7, fibroblast PTGDS–PGD2–PTGDR) for therapeutic targeting.
This work provides the first comprehensive single-cell atlas of rosacea skin across subtypes, defining 11 major cell types and multiple disease-associated subpopulations. It identifies a disease-enriched CD74+ keratinocyte population with IFNγ-driven barrier impairment, delineates immune remodeling with Th1/Th17 polarization and increased TRM cells, and details vascular alterations with impaired mural cell contractility. Crucially, fibroblasts emerge as the principal determinants of rosacea by producing pro-inflammatory chemokines and vasodilatory signals, validated functionally by fibroblast depletion and PTGDS knockdown abrogating rosacea-like phenotypes in mice. These insights prioritize fibroblast-centered pathways and IFNγ signaling as promising therapeutic avenues. Future research should expand patient cohorts (including males), integrate spatial multi-omics to map neuroimmune–vascular interactions, and explore the contributions of microbiome-driven type I IFN signaling during flares.
- Small human sample size limits generalizability; some assumptions are drawn from scRNA-seq datasets with limited numbers per condition.
- Only female human samples were analyzed; applicability to males remains to be tested.
- Healthy skin samples were dominated by keratinocytes, confounding proportion estimates for less abundant cell types; interpretations of cell-type frequencies, especially when fewer than 10 cells were captured, should be made cautiously.
- Neurons were not captured in scRNA-seq (cell bodies not in skin), limiting direct conclusions on neuronal contributions and requiring complementary spatial or proteomic approaches.
- GSEA was performed without multiple comparison adjustment for visualization, warranting cautious interpretation of pathway rankings.
Related Publications
Explore these studies to deepen your understanding of the subject.