Medicine and Health
Single-cell guided prenatal derivation of primary fetal epithelial organoids from human amniotic and tracheal fluids
M. F. M. Gerli, G. Calà, et al.
The study addresses the lack of autologous, patient-specific models of developing human tissues available during ongoing pregnancies, which limits prenatal investigation, prognostication, and therapy design for congenital anomalies. Despite sophisticated prenatal genetic and imaging diagnostics, severity prediction and patient stratification remain challenging for several conditions. Access to fetal tissues is ethically and legally restricted and generally limited to earlier gestational ages, hindering analysis of later development. The authors hypothesized that human amniotic fluid, which contains cells shed from multiple developing organs, harbors viable epithelial stem/progenitor cells that can be isolated during pregnancy and expanded into primary organoids without reprogramming. They aimed to map AF cellular content at single-cell resolution, isolate lineage-committed epithelial progenitors, and derive clonal, tissue-specific fetal organoids (intestine, kidney, lung). They further tested whether organoids derived from AF and tracheal fluid of fetuses with congenital diaphragmatic hernia (CDH) recapitulate disease features, enabling prenatal disease modeling and potentially informing personalized therapies within clinically relevant timelines.
Prior approaches for autologous organoid generation rely on embryonic stem cells or induced pluripotent stem (iPS) cells, including iPS organoids reprogrammed from AF-derived fetal cells; however, extensive manipulation and lengthy differentiation reduce patient fidelity and prenatal applicability. Primary organoids with minimal manipulation have been derived from postnatal discarded samples (urine, menstrual flow, PAP smears, bronchoalveolar lavage), and fetal organoids have been generated from postmortem biobanked tissues, but such methods are destructive and restricted by ethical/legal constraints and gestational age limits (~20–22 weeks). AF is known to contain cells and secretions from developing organs (gastrointestinal tract, kidney, lung), and also mesenchymal and hematopoietic stem cells; however, a detailed map of AF epithelial populations and their organoid-forming potential was lacking. Fetal therapeutic interventions (amniodrainage, procedures for TTTS, MMC repair, and FETO for CDH) offer access to fetal fluids during pregnancy, suggesting a route to obtain autologous cells non-destructively. This work builds on these insights to create primary fetal epithelial organoids directly from fetal fluids collected during the second and third trimesters.
Ethics: AF and tracheal fluid (TF) samples were collected after informed consent under UK and Belgian approvals (UCLH FMU REC 14/LO/0863 IRAS 133888; UZ Leuven S53548). Control fetal tissues were obtained from the HDBR with appropriate approvals.
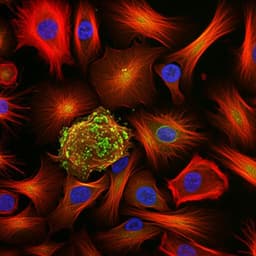
AF single-cell mapping: AF from 12 pregnancies (15–34 gestational weeks) was processed to isolate viable nucleated cells using FACS (Hoechst+/PI−, without FSC/SSC gating to preserve heterogeneity). 3' scRNA-seq libraries (10x Genomics) were generated and analyzed with CellRanger, Seurat v4 (integration, UMAP), and SingleR for epithelial cluster annotation; ambient RNA correction used CellBender. scGSEA and module scoring assessed tissue-origin signatures (gastrointestinal, kidney, lung) and progenitor markers; flow cytometry validated EpCAM and E-cadherin expression.
Organoid derivation (AFOs): Viable AF cells were embedded in Matrigel (6×10^4 cells/30 µl droplet) and cultured in a defined generic epithelial expansion medium with ROCK inhibitor for 3 days. Organoids visible by ~2 weeks were clonally picked, dissociated to single cells, and expanded as individual lines. Organoids were passaged every 10–14 days (mechanical or TrypLE dissociation), cryopreserved in 80% FBS/20% DMSO, and thawed for further expansion. Formation efficiency (P0) and area were quantified by microscopy.
TF organoids (LTFOs): TF collected during FETO (pre- and post-balloon) was processed without FACS due to small volume and high viability; cells were cultured in fetal lung organoid medium. Clonal picking and passaging matched AFO procedures.
Controls: Primary fetal tissue-derived organoids from small intestine, stomach, kidney, bladder, lung, and placenta were generated using established protocols and used as transcriptomic references.
Differentiation/maturation protocols: SiAFOs matured for 14 days in intestinal-specific medium; Notch inhibition (DAPT) or Wnt activation (CHIR99021) assessed lineage changes. KAFOs were differentiated for 14 days in distal/collecting duct medium (± aldosterone/vasopressin). LAFOs underwent proximal airway differentiation (PneumaCult ALI Medium, 14 days) or distal differentiation (reported medium, 14 days).
Functional and structural assays: SiAFO brush border enzyme activities (dipeptidyl peptidase IV, disaccharidase) were quantified; SiAFOs were assembled into ring constructs in collagen hydrogels and analyzed by microCT and IF. KAFO barrier integrity was assessed via inulin-FITC permeability (± EDTA), and potassium channel activity via FluxOR II thallium influx assay. LAFO ciliation was analyzed by IF (Ac-αTUB, FOXJ1), TEM for axoneme ultrastructure, and high-speed video to measure ciliary beat frequency (CBF). Distal lung maturation was probed by IF (SFTPB) and TEM for lamellar bodies.
Molecular profiling: Bulk RNA-seq (NextSeq 2000) of 121 AFO lines from 23 AF samples and control organoids; PCA, hierarchical clustering, and GO analyses assessed tissue identity. scRNA-seq on representative AFOs (small intestine n=3, kidney n=6, lung n=4 organoid lines) characterized cellular composition and differentiation responses; deconvolution used CellSNP-lite/Vireo. IF and flow cytometry validated marker proteins. Statistical analyses used t-tests or ANOVA with multiple comparisons; significance thresholds as specified in figures.
- AF contains viable epithelial progenitors from multiple tissues: scRNA-seq (12 AF samples; 33,934 cells post-filtering) identified an epithelial cluster expressing pan-epithelial markers (EPCAM, CDH1, KRTs). scGSEA and progenitor scoring revealed gastrointestinal, renal, and pulmonary epithelial progenitors.
- Efficient derivation of clonal AF organoids (AFOs): From 42 AF samples (16–34 weeks GA), 423 clonal AFO lines were established; 89.7% of AF samples formed organoids, with median formation efficiency 0.011% (≈1 organoid per 7.4×10^3 viable cells). AFOs expanded up to ≥P20 and were cryopreservable.
- Tissue identity confirmed: Bulk RNA-seq of 121 AFOs formed three clusters aligning with control fetal small intestine, kidney, and lung organoids; one AFO matched placenta. GO analyses supported tissue-specific pathways; scRNA-seq of AFOs showed multiple epithelial subtypes per tissue.
- Small intestine AFOs (SiAFOs): Exhibited crypt-like morphology, proliferation at crypt bases, and expressed intestinal stem/progenitor (LGR5, OLFM4, LRIG1, SMOC2), Paneth (LYZ), goblet (MUC2), enteroendocrine (CHGA), and enterocyte (ALPI, FABP1, VIL1, EZR, KRT20, ATP1A1) markers. Maturation increased budding, goblet and enteroendocrine cells, and upregulated enterocyte/goblet genes (FABP1, ALPI, MUC2) while downregulating Notch targets (HES1, OLFM4) and Wnt target AXIN2 (DAPT). Functional brush border enzyme activities (dipeptidyl peptidase IV, disaccharidase) were demonstrated. SiAFOs self-assembled into polarized, lumenized intestinal ring structures with appropriate lineages (enterocytes, Paneth, goblet, enteroendocrine) and tight junctions (ZO-1).
- Kidney tubule AFOs (KAFOs): Long-term expandable (to P10), with proliferation (Ki67) and mixed distal/proximal tubule identity: expressed PAX2, PAX8, LHX1, JAG1; distal (PCBD1, SLC41A3, POU3F3) and proximal (ABCC1/3/4, CUBN) markers; collecting duct marker GATA3 present; UMOD absent; podocyte markers largely absent (WT1, NPHS1/2 not expressed; PODXL, MAFB detected). Protein staining confirmed PAX8, LHX1, GATA3, LTL, ECAD, apical Ac-αTUB; tight junctions (ZO-1) present. Functional features included increased thallium influx (voltage-gated K+ channels) comparable to fetal kidney organoids and greater than fetal lung organoids (P=0.0393), and intact barrier function in 67.9% of KAFOs reduced to 24.4% by EDTA (P=0.0121). 21/54 lines expressed RET, associated with morphological differences. Differentiation induced AQP2, SLC12A1, and CALB1 expression (CALB1 protein increase P=0.0357; transcript P=0.0029).
- Lung AFOs (LAFOs): 43 lines from 12 AF samples (16–34 GA) expanded to P21; expressed lung progenitor/stem markers (NKX2-1, FOXA2, SOX2, SOX9, TP63, GATA6) and alveolar markers (AT1: HOPX, PDPN, AGER, AQP5; AT2: SFTPA1/2, SFTPB/C/D, ABCA3, LAMP3). In expansion, mature basal (KRT5, TROP2, NGFR) and club (SCGB1A1) markers were low/absent; proSFTPC absent. Proximal differentiation generated ciliated and deuterosomal cells with luminal motile cilia (Ac-αTUB; FOXJ1+ cells increased to 62.8±8.2% vs expansion, P=0.0016), with goblet (MUC5AC) and maintenance of SOX2; TEM showed normal axoneme ultrastructure and CBF within physiological range. Distal differentiation increased SFTPA1/2, SFTPB/D expression; SFTPB protein localized intracellularly or luminally; TEM showed lamellar bodies (immature ultrastructure). scRNA-seq indicated emergence of lower airway progenitors and Hillock-like clusters upon distalization.
- CDH disease modeling: Lung organoids derived from CDH AF (16/20, 80% success) and TF (7/17, 41.2% success) resembled controls morphologically, expressed NKX2-1, SOX2, P63, and proliferated. CDH organoids showed higher SOX9 IF positivity than controls; SOX9 decreased post-FETO (consistent with maturation). Transcriptomic differences vs GA-matched controls were greater pre-FETO (380 DEGs, P<0.01, logFC>2) than post-FETO (102 DEGs). GO analysis revealed upregulated surfactant production/metabolism and phosphatidylcholine metabolism, with downregulated ECM/integrin/laminin interactions (more evident post-FETO). proSFTPC and SFTPB were validated by IF. Proximal differentiation yielded cilia (TEM, Ac-αTUB, FOXJ1) with normal CBF; distal differentiation produced lamellar bodies. scRNA-seq showed decreased basal and club cells and increased pulmonary neuroendocrine cells in CDH organoids, with increased AT2 representation; control distalized LAFOs showed Hillock and lower airway progenitor cells absent in distalized CDH LAFOs.
The findings demonstrate that human amniotic and tracheal fluids collected during ongoing pregnancies contain viable, lineage-committed fetal epithelial progenitors capable of generating primary, clonal organoids that recapitulate small intestinal, renal tubule, and pulmonary tissue identities at transcriptomic, protein, structural, and functional levels. This directly addresses the need for autologous, minimally manipulated prenatal models, circumventing ethical and logistical constraints of fetal tissue procurement and the time-intensive iPS-based approaches. The ability to derive and expand organoids within 4–6 weeks aligns with clinical decision windows for prenatal interventions, enabling patient-specific modeling, functional assays, and potentially therapeutic testing.
Disease modeling in CDH showed organoids retain disease-relevant phenotypes, including altered surfactant pathway gene expression, higher stem/progenitor features (SOX9) pre-FETO with maturation post-FETO, reduced basal/club cells, increased pulmonary neuroendocrine and AT2-like cells, and ECM-related pathway differences—consistent with human and animal CDH lungs. These similarities suggest AFOs/LTFOs could complement prenatal prognostication and guide therapy selection. The platform also opens access to later gestational stages currently underrepresented in fetal atlases, expanding the developmental window for study.
This study establishes a pipeline for deriving autologous primary fetal epithelial organoids from amniotic and tracheal fluids during ongoing pregnancies. Single-cell mapping of AF identified gastrointestinal, renal, and pulmonary epithelial progenitors that yielded clonal organoids reflecting their tissues of origin, with demonstrated structural and functional maturation. Lung organoids from CDH AF/TF recapitulated disease-associated molecular and cellular features and captured maturation changes around FETO. The approach offers a rapid (4–6 weeks), minimally invasive, and widely applicable route to generate patient-specific prenatal models for disease investigation, counseling, and personalized regenerative medicine.
Future work should expand organoid derivation to additional AF-exposed tissues, integrate non-epithelial compartments (mesenchymal/endothelial) for more complex models, optimize cost-effective identity assays (e.g., PCR, imaging), and validate prognostic utility in larger CDH and other congenital anomaly cohorts with correlation to clinical outcomes.
- Current system models only epithelial compartments; it cannot capture mesenchymal/vascular interactions without co-culture.
- CDH analyses were limited by sample availability; paired pre/post-FETO samples were not always obtainable, and post-FETO AF sampling occurs before balloon removal, so AF-derived LAFOs may not fully reflect FETO-induced lung changes (TF-derived organoids better capture occluded-lung status).
- SiAFO derivation was rare (successful in only two AF samples at 16–17 weeks GA), limiting intestinal modeling generalizability.
- One organoid line showed mixed identity (likely non-clonal picking error).
- The AF environment introduces ambient RNA and cell stress; existing fetal atlases underrepresent late gestational stages, complicating reference-based annotations.
- Larger patient cohorts are needed to validate disease-modeling and prognostic applications.
- Platform timelines and success rates may vary with fluid volume, viability, and gestational age, and formation efficiencies at the single-cell level are low (median 0.011%).
Related Publications
Explore these studies to deepen your understanding of the subject.