Medicine and Health
Semen Ziziphi Spinosae attenuates blood-brain barrier dysfunction induced by lipopolysaccharide by targeting the FAK-DOCK180-Rac1-WAVE2-Arp3 signaling pathway
H. Liu, X. Zhang, et al.
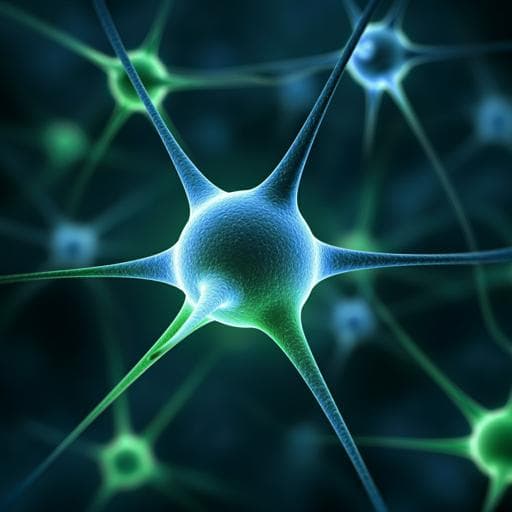
The blood-brain barrier (BBB), formed by cerebral microvessel endothelial cells connected by tight and adherens junctions and supported by pericytes and astrocytes, maintains CNS homeostasis by restricting entry of toxins and pathogens. Early BBB breakdown contributes to neurodegenerative and neuropsychiatric disorders. Semen Ziziphi Spinosae (SZS; Suanzaoren) is widely consumed in China as a functional food and used in traditional medicine for sedative and neuroprotective effects, with reported antioxidant, anti-inflammatory, and cognition-related benefits. Because oxidative stress and inflammation degrade junction proteins and impair BBB integrity, SZS might protect the BBB, yet its effects on BBB and mechanisms are unclear. LPS is a common inducer of BBB damage via oxidative and inflammatory pathways. This study investigates whether SZS protects against LPS-induced BBB dysfunction in rats and hCMEC/D3 cells, profiles cortex proteomic changes, identifies in vivo SZS components, and explores mechanisms focusing on cell adhesion/junctions and actin cytoskeleton signaling.
The authors reference evidence that BBB disruption contributes to diseases such as Alzheimer’s, Parkinson’s, and depression, and that LPS induces BBB injury via oxidative stress and inflammation (e.g., Nrf2 and NF-κB pathways). Prior work documents SZS’s antioxidant, anti-inflammatory, anxiolytic, and cognition-improving effects, and active constituents such as spinosin. Cytoskeletal regulation of endothelial junctions via Rac1–WAVE2–Arp2/3 and upstream factors (FAK, DOCK180) is implicated in BBB permeability, yet LPS-induced BBB damage via the FAK–DOCK180–Rac1–WAVE2–Arp3 pathway and SZS’s role had not been reported. This study addresses these gaps.
In vivo: Forty Sprague–Dawley rats (male/female, 200 ± 20 g) were acclimatized and randomized into four groups: control (CON), LPS, SZS, and positive control (POS). SZS group received SZS decoction orally (2 g/kg/day) for 30 days; POS received vitamin C (Vc, 0.2 g/kg/day); CON and LPS received water. Except CON, rats were injected intraperitoneally with LPS (10 mg/kg); 12 h later animals were anesthetized for sample collection. Assessments included: histology (H&E, Nissl, TUNEL), transmission electron microscopy of cortex ultrastructure, BBB permeability by Evans blue (2% EB, 2 mg/kg i.v.; fluorescence quantification), biochemical assays in cortex and plasma for oxidative stress (SOD, GSH, MDA, H2O2, ROS, protein carbonyls) and inflammation (IL-6, TNF-α) using commercial kits, and western blotting (normalized to total protein) for junction proteins (ZO-1, occludin, E-cadherin, β-catenin), P-glycoprotein (P-gp), actin polymerization (F-/G-actin ratio), and signaling proteins (FAK, DOCK180, Rac1, WAVE2, Arp3). For proteomics, cortex proteins (six biological replicates per group for CON, LPS, SZS) were processed by trypsin digestion and analyzed by NanoElute LC coupled to TIMS-TOF MS. Protein identification used Peaks Online against Swiss-Prot (Rattus norvegicus), with DEPs defined at fold change >1.4 or <0.71 and P < 0.05. Functional annotation used DAVID; expression trends were clustered (Mfuzz). In vitro: hCMEC/D3 cells were cultured in RPMI-1640 with 10% FBS. Groups: CON, LPS, low-/mid-/high-dose SZS (50, 100, 200 µg/mL), and POS (Vc 50 µg/mL). Cells were preincubated with SZS or Vc for 24 h, then exposed to LPS (10 µg/mL) for 24 h (except CON). Outcomes: apoptosis by flow cytometry (Annexin V-FITC/PI), monolayer paracellular permeability by sodium fluorescein flux, TEER measurement, immunofluorescence for F-actin (phalloidin) and junction proteins (occludin, ZO-1, E-cadherin), and western blotting for junction and signaling proteins and F-/G-actin ratio. Chemical profiling: UPLC-HR-MS (Orbitrap Fusion Lumos) characterized SZS decoction constituents and in vivo plasma prototypes after SZS dosing, using standards (e.g., spinosin, swertisin, 6''-feruloylspinosin, coclaurine, etc.). Molecular docking: in vivo-identified SZS compounds were docked to pathway proteins (FAK, DOCK180, Rac1, WAVE2, Arp3) using AutoDock 4.2 (LibDock protocol) with docking scores and molecular dynamics simulations to assess binding modes.
- Morphology/ultrastructure: LPS caused cortical inflammation, nuclear shrinkage, cell swelling, decreased Nissl bodies, and increased apoptosis; SZS restored morphology and reduced apoptosis. In hCMEC/D3 cells, SZS (50–200 µg/mL) reduced LPS-induced apoptosis from 29.1% (LPS) to 18.4%, 17.0%, and 15.9% (dose-dependent). TEM showed that SZS repaired LPS-induced ultrastructural damage, narrowing intercellular space, reducing astrocyte swelling, and restoring mitochondrial integrity.
- BBB permeability: LPS increased Evans blue extravasation; SZS reduced EB content by 52.5% vs LPS, Vc by 33.5%. In hCMEC/D3 monolayers, high-dose SZS (200 µg/mL) decreased sodium fluorescein permeability by 16.0% (P < 0.01) and increased TEER by 53.5% (P < 0.05); medium dose also improved permeability and TEER; low dose had no significant effect.
- Oxidative stress and inflammation: In rats, SZS increased cortical GSH and reduced ROS, MDA, H2O2, and protein carbonyls compared with LPS; plasma GSH and SOD trends improved. IL-6 and TNF-α elevated by LPS in cortex and plasma were reduced by SZS. In hCMEC/D3 cells, SZS dose-dependently decreased IL-6, TNF-α, MDA, H2O2, and ROS.
- Junction proteins and P-gp: In rat cortex, LPS decreased occludin, β-catenin, and P-gp; SZS elevated β-catenin (P < 0.05) and tended to restore occludin and P-gp; ZO-1 unchanged. In hCMEC/D3, LPS reduced all TJ/AJ proteins and P-gp; SZS significantly upregulated ZO-1 (P < 0.01) and β-catenin dose-dependently; 200 µg/mL SZS increased E-cadherin by 9.07% and P-gp by 19.9% (P < 0.05). IF showed improved expression/distribution of occludin and ZO-1.
- Proteomics: 3,998 proteins identified. DEPs: LPS/CON=387; SZS/LPS=135. LPS altered proteins enriched in cell-cell adhesion, GTP/GDP binding, and intermediate filament/neurofilament organization. SZS modulated proteins associated with dendritic shaft/spine, postsynaptic density/membrane, and cell junctions. Clustering showed SZS reversed LPS-induced downregulation (Clusters 1–2; e.g., cadherin binding/cell-cell adhesion) and reduced LPS-upregulated proteins (Clusters 3–4; GTPase activator activity, Rab GTPase binding). Western validation (e.g., CYP2D1) matched MS trends.
- FAK–DOCK180–Rac1–WAVE2–Arp3 pathway and actin dynamics: LPS decreased cortical FAK, DOCK180, Rac1, and F-/G-actin ratio; SZS increased FAK (+41.2%, P < 0.01), DOCK180 (+44.4%, P < 0.05), Rac1 (+6.7%, P < 0.01), WAVE2 (+32.5%, P < 0.01), Arp3 (+64%, P < 0.05), and restored F-/G-actin ratio (P < 0.01). In hCMEC/D3, LPS reduced FAK (−22.1%), DOCK180 (−47.3%), WAVE2 (−10.5%), Arp3 (−61.4%), and F-/G-actin (−66.3%); SZS dose-dependently increased DOCK180, Rac1, Arp3, F-/G-actin, and at high dose increased WAVE2; all doses increased FAK. IF showed SZS restored F-actin expression/distribution.
- Chemical profiling and docking: UPLC-HR-MS identified 33 decoction constituents and 13 in vivo plasma compounds; prototypes SPI, SWE, FSP, and others were confirmed. Docking indicated 6''-feruloylspinosin (FSP), spinosin (SPI), and swertisin (SWE) had the most favorable binding to FAK, DOCK180, Rac1, and Arp3, forming multiple hydrogen bonds; WAVE2 showed relatively lower binding affinity due to structural features. Molecular dynamics supported stable binding, with FSP generally exhibiting the lowest docking energies among targets.
The study demonstrates that SZS mitigates LPS-induced BBB dysfunction by attenuating oxidative stress and inflammation, preserving junctional complexes (ZO-1, occludin, E-cadherin, β-catenin) and P-gp, and stabilizing the actin cytoskeleton. Proteomics revealed that LPS disrupts cell adhesion and cytoskeletal organization, consistent with increased BBB permeability and ultrastructural changes, while SZS restores proteins linked to cell junctions and synaptic structures. Mechanistically, SZS activates the FAK–DOCK180–Rac1–WAVE2–Arp3 axis to promote actin polymerization (increased F-/G-actin ratio), reinforcing endothelial contacts and barrier integrity. Chemical analyses and docking suggest that in vivo-absorbed flavone C-glycosides (FSP, SPI, SWE) may directly interact with pathway proteins, providing a plausible molecular basis for SZS’s effects. These findings extend BBB-protective mechanisms beyond commonly studied NF-κB/Nrf2 or RhoA/ROCK pathways and imply that SZS could confer neuroprotection in conditions where BBB breakdown is an early pathophysiological event.
This work provides the first evidence that Semen Ziziphi Spinosae prevents LPS-induced BBB dysfunction by upregulating the FAK–DOCK180–Rac1–WAVE2–Arp3 signaling pathway, enhancing actin polymerization, and restoring tight/adherens junction proteins and P-gp. Proteomics supports SZS-mediated normalization of cell adhesion and cytoskeletal networks, and chemical/docking analyses implicate in vivo constituents (6''-feruloylspinosin, spinosin, swertisin) as potential pathway interactors. SZS emerges as a promising neuroprotective functional food targeting BBB integrity. Future studies should validate the causal role of the identified pathway using specific inhibitors or genetic tools, assess individual active compounds in vivo, explore pharmacokinetics and bioavailability, and evaluate efficacy in disease-relevant models with behavioral outcomes.
- The BBB injury model is limited to LPS-induced acute inflammation; generalizability to other BBB-disruptive pathologies requires validation.
- Mechanistic inference relies on correlative protein expression and docking; direct causal evidence (e.g., pathway inhibition/knockdown) was not provided.
- Docking and molecular dynamics suggest interactions but do not confirm in vivo target engagement; active compounds’ BBB penetration and exposure-response relationships were not fully defined.
- Jujubosides, known bioactives, were not detected in plasma (low bioavailability), leaving uncertainty about contributions of other constituents.
- Behavioral or functional neurological outcomes were not assessed; sample sizes for some assays were modest (e.g., n=6 for proteomics, n≈9 for biochemistry/western).
Related Publications
Explore these studies to deepen your understanding of the subject.