Medicine and Health
SARS-CoV-2 infection of human lung epithelial cells induces TMPRSS-mediated acute fibrin deposition
R. Erickson, C. Huang, et al.
Discover groundbreaking research by Rachel Erickson and colleagues on a novel fibrin clotting mechanism linked to severe COVID-associated lung injury. This study reveals how SARS-CoV-2 infection in primary lung cells triggers fibrin formation and highlights the limitations of current anticoagulation treatments, making a compelling case for developing new therapeutic strategies.
~3 min • Beginner • English
Introduction
The study addresses how SARS-CoV-2 infection contributes directly to fibrin deposition and diffuse alveolar damage (DAD) in COVID-19 lungs. Although COVID-19 is associated with thrombotic events and hyaline membrane formation typical of ARDS, and anticoagulation with heparin is standard-of-care, mortality remains high and mechanisms of lung fibrin deposition are unclear. The authors hypothesize that SARS-CoV-2 infection of lung epithelial cells triggers a non-classical, cell-mediated fibrin clotting process within the alveolar space, independent of the traditional tissue factor-driven plasma coagulation pathway. They aim to define whether infected airway epithelial cells can directly drive fibrin formation, identify the responsible proteases, and evaluate implications for therapy.
Literature Review
Background autopsy and clinical studies show extensive DAD and fibrin microthrombi in COVID-19 lungs, with thrombotic structures in pulmonary vessels and elevated D-dimer in severe cases. ARDS-related hyaline membranes and fibrinous deposits have been attributed to classical extrinsic coagulation (tissue factor–initiated) and fibroproliferative pathways (e.g., TGF-β), with additional proposed roles for neutrophil extracellular traps. Prior reports indicated inflammatory infiltrates in BAL and possible upregulation of tissue factor in infected epithelium. However, whether viral infection per se drives fibrin deposition in alveolar spaces, distinct from vascular coagulation, remained unresolved.
Methodology
- Human samples: Bronchoalveolar lavage fluid (BALF) from healthy donors and COVID-19 patients (acute within a week of symptom onset; recovered >30 days post-discharge). Proteomics by LC-MS/MS performed on 3 healthy, 4 acute, and 4 recovered BALF samples; ELISAs (fibrinogen, prothrombin, total IgG) on 15 healthy, 4 acute, and 7 recovered BALF samples.
- Cell models: Primary normal human bronchial/tracheal epithelial cells (NHBE), human small airway epithelial cells (HSAEC), ACE2-expressing 293T, HEK293T, and Vero E6 cells. NHBE also cultured at air–liquid interface (ALI) for infection with replication-competent viruses.
- Viral infections: SARS-CoV-2 pseudoviruses (HIV-luciferase core) bearing spike proteins from Wuhan, Alpha, Beta, Gamma, Delta, Omicron. Replication-competent strains (WA-1, Alpha, Beta, Delta) used at MOI 3 for NHBE ALI cultures.
- Fibrin clotting assays: Turbidity-based assays at 350 nm to monitor fibrin formation after adding fibrinogen to infected or uninfected cells and/or supernatants. Positive control: thrombin-induced clotting. Confocal microscopy with TAMRA-labeled fibrinogen and SEM to visualize fibrin network.
- Thrombin dependence and inhibitors: Assessed infection-induced clotting in presence of serine protease inhibitor camostat, thrombin-specific inhibitor hirudin, and direct thrombin inhibitors dabigatran and argatroban. Mass spectrometry of culture supernatants to detect thrombin; depletion of bovine prothrombin from media and rescue with purified human prothrombin to confirm thrombin dependence and human prothrombin compatibility.
- Prothrombin activation assays: Fluorogenic peptide corresponding to prothrombin factor Xa cleavage site (Thrb-324) to test cleavage by Factor Xa, infected vs. uninfected NHBE supernatants, and recombinant proteases. Thrombin activity assessed via cleavage of an N-terminal fibrinogen-β fluorogenic peptide; inhibition by dabigatran verified specificity.
- Transcriptomics and gene perturbation: RNA-seq on NHBE/HSAEC infected with pseudovirus or Delta field strain to profile interferon response, tissue factor (F3), and TMPRSS genes. CRISPR/Cas9 RNP-mediated knockdown of tissue factor (F3) in NHBE and HSAEC; western blot confirmation and subsequent clotting assays to test TF independence.
- TMPRSS involvement: Expression profiling (RNA-seq TPM and western blots) for ST14 (matriptase) and TMPRSS11D (HAT) across cell types. Western blot detection of matriptase shedding into supernatant after infection. Use of metalloproteinase inhibitors (BB-94, prinomastat) during infection to assess impact on protease shedding and downstream clotting (control experiments adding inhibitors only during clotting to exclude direct effects). Component assays mixing human prothrombin and fibrinogen with recombinant matriptase or HAT versus Factor Xa. Gain-of-function: transfection of ST14 or TMPRSS11D into ACE2-293T cells followed by pseudovirus infection and clotting assay.
- Ex vivo BALF clotting: Healthy, acute COVID, and recovered COVID BALF were dialyzed, concentrated 20× to approximate epithelial lining fluid, and tested for fibrin clotting in the presence of infected or uninfected NHBE cells with/without exogenous fibrinogen supplementation.
- Statistics: Mostly two-sided unpaired t-tests and two-way ANOVA where indicated; p-values commonly <0.0001. Imaging and assays replicated as described.
Key Findings
- Proteomics and ELISA of BALF:
- Acute COVID BALF showed increased infiltration of plasma proteins, complement components, and coagulation factors compared with healthy and recovered samples.
- Prothrombin and fibrinogen were elevated ~50–100-fold in acute BALF versus healthy (ELISA); recovered levels were similar to healthy.
- Infection-induced fibrin formation:
- SARS-CoV-2 pseudovirus or replication-competent strains induced fibrin clotting in infected NHBE and HSAEC but not in uninfected cells; no clotting in infected Vero E6 or ACE2-293T unless TMPRSS genes were overexpressed.
- Fibrin fibers originated from infected NHBE cell surfaces, consistent with a cell-mediated mechanism; robust networks observed by confocal and SEM.
- Spike binding alone (soluble spike, S1, or RBD) did not induce clotting; infection was required.
- Effect observed across spikes from multiple variants (Wuhan, Alpha, Beta, Gamma, Delta, Omicron) and with field strains (WA-1, Alpha, Beta, Delta).
- Thrombin dependence and source:
- Camostat and thrombin inhibitors (hirudin, dabigatran, argatroban) abolished infection-induced fibrin clotting (p < 0.0001).
- Mass spectrometry identified bovine thrombin in infected supernatants; depleting bovine prothrombin abrogated clotting, which was restored by adding human prothrombin, demonstrating thrombin dependence with human prothrombin.
- Prothrombin activation by infected cells:
- Infected NHBE supernatants alone induced fibrin clotting and cleaved the prothrombin Thrb-324 peptide more than uninfected supernatants; thrombin activity confirmed by cleavage of fibrinogen-β peptide and inhibited by dabigatran.
- Independence from classical TF pathway:
- RNA-seq showed interferon/antiviral responses but no significant upregulation of tissue factor (F3) in infected NHBE/HSAEC.
- CRISPR knockdown of tissue factor did not prevent infection-induced fibrin formation, indicating TF independence.
- TMPRSS proteases implicated:
- NHBE/HSAEC expressed ST14 (matriptase) and TMPRSS11D (HAT); these were absent in Vero and 293T.
- Infection caused shedding of matriptase; metalloproteinase inhibitors (BB-94, prinomastat) during infection reduced subsequent clotting, consistent with reduced shedding/activation.
- Recombinant matriptase and HAT cleaved the Thrb-324 peptide and, when combined with human prothrombin and fibrinogen, promoted fibrin clotting similar to Factor Xa.
- Overexpression of ST14 or TMPRSS11D in ACE2-293T enabled infection-induced fibrin formation.
- Ex vivo BALF findings:
- Infected NHBE cells triggered or enhanced fibrin clotting in 3 of 4 acute COVID BALF samples without added fibrinogen; healthy BALF required exogenous fibrinogen to see clotting in some cases; most recovered BALF did not clot unless infected and with higher residual fibrinogen/prothrombin.
- One acute sample (C3146) did not form clots despite elevated fibrinogen, suggesting countervailing fibrinolytic/anticoagulant factors (e.g., plasminogen, antithrombin III).
Discussion
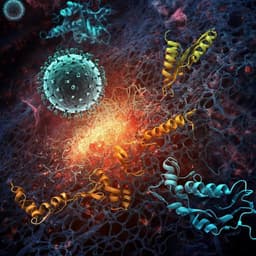
Findings support a non-classical, cell-mediated thrombin activation and fibrin deposition mechanism within the alveolar airspaces of SARS-CoV-2–infected lungs. Rather than relying on vascular leakage and tissue factor–driven plasma coagulation, infection of airway epithelial cells activates and sheds TMPRSS family proteases (e.g., matriptase/ST14, HAT/TMPRSS11D) that exhibit Factor Xa–like activity, cleaving prothrombin into thrombin. Resultant thrombin then cleaves fibrinogen to produce fibrin networks originating at epithelial surfaces. Elevated prothrombin and fibrinogen in acute COVID BALF increase the risk for this airway fibrin deposition, aligning with histopathological observations of hyaline membranes and fibrinous DAD. The thrombin dependence and efficacy of direct thrombin inhibitors (hirudin, dabigatran, argatroban) indicate that targeting airway thrombin may mitigate pathology. Because this mechanism is extra-vascular and independent of tissue factor, standard heparin-based anticoagulation (primarily targeting Factor Xa in the bloodstream) may be less effective against airway fibrin formation. Results across multiple variants and replication-competent viruses suggest this is a generalizable feature of SARS-CoV-2 infection in lung epithelium.
Conclusion
The study identifies a SARS-CoV-2 infection–induced, TMPRSS-mediated pathway for prothrombin activation and fibrin deposition in the alveolar space, independent of the classical tissue factor–driven coagulation cascade. Primary human lung epithelial cells (NHBE/HSAEC), upon infection, shed/activate matriptase (ST14) and HAT (TMPRSS11D), which can directly activate prothrombin to thrombin, producing fibrin clots that are inhibited by direct thrombin inhibitors. Elevated prothrombin and fibrinogen in acute COVID BALF, combined with infected epithelial cells, potentiate fibrin formation ex vivo. Clinically, these findings help explain limited efficacy of systemic heparin in preventing COVID-associated lung damage and suggest inhaled/nebulized direct thrombin inhibitors as a targeted therapeutic strategy. Future research should develop and employ suitable viral ARDS animal models to test airway-directed thrombin inhibition in vivo, delineate regulation of TMPRSS activation/shedding, and map patient-specific procoagulant versus fibrinolytic factors that modulate risk.
Limitations
- The core evidence is derived from in vitro primary epithelial cell models and ex vivo BALF assays; in vivo validation is lacking due to limited animal models that recapitulate COVID-19 ARDS/DAD.
- Not all acute COVID BALF samples formed clots despite elevated fibrinogen, indicating patient-to-patient variability and influence of fibrinolytic/anticoagulant factors (e.g., plasminogen, antithrombin III, SERPINs) not fully characterized here.
- The precise in vivo dynamics and localization of TMPRSS protease shedding/activation and the balance with endogenous inhibitors were not directly measured in patients.
- While bovine prothrombin in culture media was controlled and human prothrombin rescue demonstrated, exact physiological concentrations and kinetics in the human lung environment may differ.
Related Publications
Explore these studies to deepen your understanding of the subject.