Medicine and Health
saRNA vaccine expressing membrane-anchored RBD elicits broad and durable immunity against SARS-CoV-2 variants of concern
M. Komori, T. Nogimori, et al.
Discover the potential of a self-amplifying RNA vaccine that offers robust protection against SARS-CoV-2 variants! This groundbreaking research demonstrates how the saRNA RBD-TM vaccine elicits strong immune responses in non-human primates and hamsters, with lasting antibody levels against variants for at least a year. Research conducted by Mai Komori and colleagues points to a promising future for durable immunity against evolving strains of the virus.
~3 min • Beginner • English
Introduction
SARS-CoV-2 has spread rapidly and globally, causing significant morbidity, mortality, and socioeconomic disruption. Continued viral evolution has produced variants of concern (VOCs) with antigenic changes that can erode vaccine-induced protection. While several COVID-19 vaccines have reduced the pandemic’s impact, their immune responses may wane relatively quickly, and breadth against evolving variants can be limited. The study aims to develop and characterize a self-amplifying RNA (saRNA) vaccine that expresses a membrane-anchored receptor binding domain (RBD-TM) of the SARS-CoV-2 spike to focus immunity on key neutralizing epitopes and elicit broad, durable protection across VOCs. The work evaluates immunogenicity, cellular responses, protective efficacy, and durability in mice, hamsters, and non-human primates (NHPs).
Literature Review
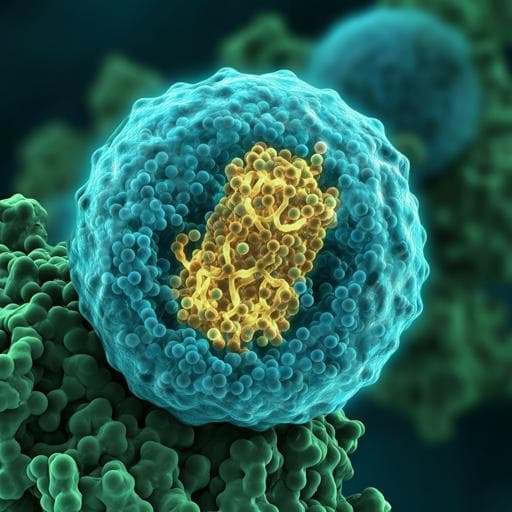
The authors reference prior development of self-amplifying RNA (saRNA) and replication RNA vaccine platforms based on alphaviruses (e.g., VEEV replicon) demonstrating potent immunogenicity at lower doses in preclinical models. They highlight evidence that a majority (>90%) of neutralizing antibodies from convalescent individuals target the spike RBD, underscoring RBD-focused vaccine designs. Prior studies demonstrated robust immune responses and protection with saRNA COVID-19 vaccine candidates in mice and NHPs, and mapped neutralizing and immunodominant epitopes on RBD. They also discuss how antigen presentation format (multivalent or membrane presentation) can enhance B cell activation, and potential issues with non-neutralizing antibodies against other spike domains contributing to inflammation. This background motivates a membrane-anchored RBD approach to enhance immunogenicity, focus on neutralizing epitopes, and improve breadth and durability against variants.
Methodology
Vaccine design and platform: A self-amplifying RNA (saRNA; also termed sarRNA) vector based on Venezuelan equine encephalitis virus (VEEV) TC-83 replicon was used, expressing alphavirus nonstructural proteins nsP1–4 for in situ RNA amplification and robust antigen expression. The antigen encodes an optimized SARS-CoV-2 spike RBD fused to an N-terminal signal peptide and a C-terminal transmembrane (TM) domain (from influenza HA) to anchor RBD on the cell membrane (RBD-TM). Secreted RBD constructs and whole spike prefusion S2P controls were also generated for comparison. Plasmid construction employed synthesized sequences and Sanger sequencing verification.
Lipid nanoparticle formulation: In vitro transcribed, capped saRNA (unmodified nucleotides) was formulated into LNPs using GenVoy-LNP/NanoAssemblr or a microfluidics method (aqueous saRNA at pH 4 mixed with ethanol lipid solution; ionizable lipid, phospholipid, cholesterol, PEG-lipid; particle size ~120–130 nm).
Animals and immunization:
- Mice (BALB/c females, typically n=5/group) received intramuscular injections of 1–10 µg saRNA-LNP at weeks 0 and 4. Comparators included protein subunit (S protein + alum) or mRNA-LNP encoding S2P.
- Hamsters (Golden Syrian, n=6/group) received 10 µg saRNA-LNP (RBD Wuhan-Hu-1 or RBD Gamma) at weeks 0 and 4, then were challenged on Day 56 with SARS-CoV-2 Wuhan-Hu-1 or Gamma; weight monitored up to 8 days post-challenge.
- Non-human primates (cynomolgus macaques; typically n=5–6/group) received 45–50 µg saRNA-LNP (RBD Wuhan-Hu-1 or RBD Gamma) at weeks 0 and 4. Challenge with Wuhan-Hu-1 SARS-CoV-2 was performed on Day 56 via intranasal/intratracheal routes. Longitudinal immunogenicity and durability were followed to week 52.
Viruses and assays: Clinical isolates included D614G, Gamma (P.1), Delta (B.1.617.2), and Omicron subvariants (BA.1, BA.2; BA.5 for select assays). Binding antibody titers were measured by ELISA against variant RBDs; surrogate ACE2-blocking activity by competitive ELISA; neutralization assessed by live-virus neutralization on VeroE6/TMPRSS2 cells (TCID50-based readouts) and pseudovirus neutralization (pVNT50). Infectious viral loads in NHP samples (BAL, nasal, oropharyngeal) post-challenge were quantified by TCID50.
Cellular immunology: Antigen-specific B cells were quantified using biotinylated RBD probes and flow cytometry in mice and NHP lymph nodes/PBMCs. T cell responses were profiled by intracellular cytokine staining following stimulation with RBD peptide pools, measuring CD4+ Th1 cytokines (IFN-γ, TNF-α, IL-2), polyfunctionality, and CD8+ T cell activation markers (CD69, CD107a) and cytokines. Th subset phenotyping (Th1/Th2/Th17, Tfh) and correlations between CD4+ activation (CD154+) and B cell responses were assessed.
Durability analysis: Antibody titers were followed to 52 weeks post-prime in NHPs. Antibody half-lives were estimated using a power-law decay model (analysis from week 12 onward) implemented in R (lme4), accounting for the week-4 boost via time offset.
Statistics: Group comparisons used Mann–Whitney U, Wilcoxon matched-pairs tests, one- or two-way ANOVA as appropriate; correlations by Spearman’s rank; significance threshold p<0.05. All animal work complied with institutional IACUC and BSL-3 requirements for live-virus work.
Key Findings
- Vaccine concept: A saRNA vaccine encoding a membrane-anchored RBD (RBD-TM) focuses immune responses on neutralizing epitopes, with higher and longer antigen expression than conventional mRNA.
- Mouse immunogenicity:
• RBD-TM saRNA (10 µg) elicited significantly higher anti-RBD IgG titers than protein subunit (10 µg S + alum) across time points (4 weeks post-prime and 2 weeks post-boost).
• Broad binding across RBD variants (K417N, E484K, N501Y) and VOC RBDs (Alpha, Beta, Delta).
• ACE2 inhibition titers were markedly higher versus S protein + alum across variants: 17.2-fold (Wuhan-Hu), 52.9-fold (Alpha), 23.9-fold (Beta), 27.4-fold (Gamma).
• Live-virus neutralization against D614G (and Gamma) was significantly higher with saRNA RBD-TM than S protein + alum; neutralizing-to-binding antibody ratio was superior to S1 subunit.
• Compared on the same saRNA platform, RBD-TM induced stronger binding responses than prefusion S2P saRNA.
- B cell responses: RBD-TM saRNA induced higher frequencies of RBD-binding memory B cells than saRNA secreted RBD or mRNA S2P (approx. 4–7-fold vs secreted RBD; ~4-fold vs mRNA S2P). Cross-binding to VOC RBDs was observed.
- T cell responses: Both saRNA vaccines (RBD-TM and secreted RBD) generated stronger Th1-skewed CD4+ responses than mRNA S2P across Wuhan-Hu-1, Beta, and Omicron, with greater IFN-γ production and increased polyfunctional CD4+ T cells (IFN-γ+TNF+IL-2+). Robust CD8+ responses (CD69, IFN-γ, TNF; CD107a/IFN-γ/TNF polyfunctionality) were induced, including cross-reactivity to Delta and Omicron. Th1 CD4 responses correlated with anti-RBD IgG titers.
- Hamster efficacy and cross-neutralization: A Gamma RBD-TM saRNA induced significantly higher neutralization titers against Gamma and Omicron BA.1 than Wuhan-Hu-1 RBD-TM, with comparable titers against D614G and BA.2. Upon challenge, both Wuhan-Hu-1 and Gamma RBD-TM vaccines prevented weight loss against homologous Wuhan-Hu-1; against Gamma challenge, Gamma RBD-TM prevented weight loss, while Wuhan-Hu-1 RBD-TM showed moderate loss; placebo animals had marked losses (up to −15%).
- NHP immunogenicity and protection: Two-dose 45–50 µg saRNA RBD-TM regimens elicited high binding titers across VOC RBDs. Vaccinated NHPs were protected upon Wuhan-Hu-1 challenge, with reduced infectious virus in respiratory samples (BAL, nasal, oropharyngeal).
- Durability in NHPs (52 weeks): Gamma RBD-TM induced higher RBD-specific IgG than Wuhan-Hu-1 RBD-TM at week 6 and maintained advantages at week 28. Estimated binding antibody half-lives: for Wuhan-Hu-1 RBD-TM, 178.5 days (Wuhan-Hu-1) and 149.9 days (Gamma); for Gamma RBD-TM, 198.4 days (Wuhan-Hu-1) and 112.7 days (Gamma). Neutralization titers for Gamma RBD-TM were sustained from week 28 to 52; live BA.5 neutralization at week 52 was detected in only one animal.
- Immunobiology in NHP nodes/blood: Vaccination activated CD4+ Th cells and induced RBD-binding IgG+ B cells in lymph nodes; CD154+ CD4+ memory T cell frequency correlated with RBD-binding CD27+IgG+ B cells. Longitudinally, antigen-specific B cells in PBMCs were higher after Gamma RBD-TM at multiple time points (weeks 10, 18, 28).
Discussion
The membrane-anchored RBD saRNA vaccine design concentrates immune responses on the RBD, which harbors most neutralizing epitopes, potentially reducing induction of non-neutralizing antibodies to other spike regions that may contribute to inflammation. The saRNA platform enhances antigen expression and duration, leading to robust humoral and cellular immunity. Across mice, hamsters, and NHPs, RBD-TM elicited strong, Th1-biased CD4+ responses with polyfunctionality, robust CD8+ responses, and broad B cell memory, translating into significant cross-reactive binding and neutralization against multiple VOCs. Protective efficacy was demonstrated in both hamster and NHP challenge models. Importantly, antibody responses were durable over 12 months in NHPs with estimated half-lives on the order of 4–6 months depending on antigen/variant pairing, and Gamma RBD-TM improved breadth against variants compared to Wuhan-Hu-1 RBD-TM. These data support the hypothesis that focusing antigen presentation to a membrane-anchored RBD via saRNA can achieve broad and durable immunity suitable for addressing evolving SARS-CoV-2 variants and may facilitate dose-sparing due to saRNA’s amplification. The platform’s flexibility also allows rapid updating with variant RBD sequences to maintain coverage against emerging strains.
Conclusion
This study demonstrates that a self-amplifying RNA vaccine encoding a membrane-anchored SARS-CoV-2 RBD (RBD-TM) induces potent, broad, and durable humoral and cellular immunity in mice, hamsters, and non-human primates, and confers protection in animal challenge models. The Gamma RBD-TM variant further enhances cross-reactive immunity and protection against variant challenges. Binding antibody responses persist for at least 52 weeks in NHPs with favorable half-life estimates, and neutralization is maintained over time for homologous/closely related strains. These findings position saRNA RBD-TM as a promising vaccine candidate for combating current and future SARS-CoV-2 variants. Future work should evaluate safety and efficacy in human clinical trials, optimize antigen selection with updated/consensus RBDs for emergent variants, assess heterologous prime-boost strategies, and explore correlates of durable protection against highly immune-evasive lineages (e.g., Omicron sublineages).
Limitations
- Human clinical data are absent; findings are from preclinical mouse, hamster, and NHP models, which may not fully predict human immunogenicity, durability, or efficacy.
- Neutralization breadth against highly immune-evasive variants is limited: live-virus neutralization of Omicron BA.5 at 52 weeks was detected in only one NHP, indicating reduced activity against some contemporary variants.
- Some datasets are from small group sizes typical of preclinical studies, potentially limiting statistical power and generalizability.
- Direct head-to-head comparisons with authorized mRNA vaccines were limited in scope and may not reflect performance with nucleoside-modified mRNA or optimized formulations used clinically.
- Mapping of protective correlates and mechanistic links between specific T cell subsets and long-term antibody maintenance requires further validation.
Related Publications
Explore these studies to deepen your understanding of the subject.