Medicine and Health
Rosmarinic acid suppresses tau phosphorylation and cognitive decline by downregulating the JNK signaling pathway
S. Yamamoto, T. Kayama, et al.
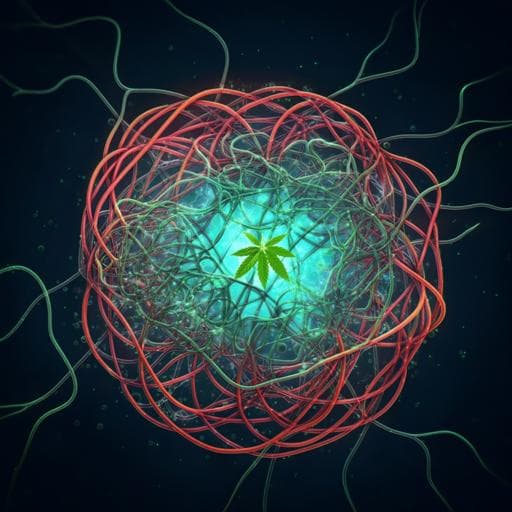
Alzheimer’s disease is marked by extracellular Aβ plaques and intracellular neurofibrillary tangles of hyperphosphorylated tau, leading to progressive dementia. Current drugs offer symptomatic relief without cure, motivating interest in preventive food components. Epidemiological evidence links polyphenol-rich diets with reduced AD risk. Rosmarinic acid (RA), abundant in Lamiaceae herbs, strongly inhibits Aβ aggregation and synaptic toxicity in vitro and has mitigated Aβ oligomerization in AD mouse models. However, whether RA affects tau phosphorylation, a key correlate of cognitive decline, and cognitive dysfunction in vivo remained unclear, especially since in vitro inhibitory concentrations exceed expected brain levels, suggesting different in vivo mechanisms. The study aimed to characterize RA’s preventive mechanisms in AD using 3×Tg-AD mice to evaluate RA’s effects on cognition, Aβ and p-tau pathology, and hippocampal transcriptomics, with a focus on pathways linked to tau phosphorylation.
Prior work indicates polyphenol-rich diets are associated with lower AD risk. RA directly binds Aβ β-sheet structures and inhibits aggregation in vitro and alleviates synaptic toxicity. RA-supplemented diet inhibited Aβ oligomerization in Tg2576 mice and suppressed tau aggregation under chronic restraint stress, though the molecular mechanism in vivo was unclear. Many structure-based in vitro mechanisms for RA’s effects on Aβ/tau use concentrations higher than achievable in brain, implying alternative in vivo modes of action. JNK signaling has been implicated in AD pathogenesis and tau phosphorylation; JNK3, predominant in the nervous system, is upregulated in AD and correlates with cognitive decline. Anti-inflammatory strategies may delay AD onset; RA exhibits anti-inflammatory activity in peripheral models, and peripheral inflammation can exacerbate central neuroinflammation and AD pathology.
- Animals and diets: Male 3×Tg-AD mice (APPswe, tauP301L, PS1M146V), 6–8 weeks old, were assigned to control diet (AIN-93G; n=8) or RA diet (AIN-93G + 0.5% RA; n=9). Housing conditions were standard with ad libitum access to food and water. Body weight and food intake were recorded twice weekly. After 8 months of feeding, mice were sacrificed; blood and organs collected under isoflurane. Ethics approval P16-224 (University of Tokyo).
- Plasma biochemistry: EDTA plasma analyzed for 12 parameters (AST, ALT, LDH, CK, TAG, free/esterified cholesterol, LDL/HDL, glucose, glycoalbumin, total ketone bodies).
- Behavioral assessments (at 10 months of age):
- Y-maze spontaneous alternation: 8-min trial in acrylic Y-maze; alternation (%) = alternations/(total entries−2). Locomotor activity inferred from total arm entries.
- Novel Object Recognition Test (NORT): Two phases (acquisition and test) 5 min each in a large cage. Intervals of 5 min and 24 h assessed short- and long-term memory. DI = (time with novel − familiar)/(total exploration time). Objects pre-validated for no innate preference.
- Immunohistochemistry (IHC): Paraffin-embedded brain sections (5 μm) processed with antigen retrieval and stained with primary antibodies: anti-Aβ 17–24 (4G8, 1:1000), anti-PHF-tau pSer202/Thr205 (AT8, 1:1000), anti-p-JNK (G-7, 1:50), anti-p-c-Jun (KM-1, 1:300). Visualization via HRP/DAB and hematoxylin counterstain. Quantifications: Aβ plaque area per 1000 μm² in cortical regions near amygdala (n=3/group). For hippocampus, CA1 and dentate gyrus (DG) subdivided into three areas; p-tau-positive cells expressed as % of total cells (n=3/group). p-JNK and p-c-Jun positive cell ratios quantified similarly.
- Hippocampal transcriptomics: Total RNA isolated (RIN>7). Affymetrix Mouse Genome 430 2.0 arrays on pooled RNA from four mice per group (average weight). Data normalized with FARMS; DEGs identified by rank product (FDR 0.05). GO and KEGG enrichment via DAVID with p<0.005 and fold enrichment >3.0 for GO; p<0.02 and fold enrichment >2.7 for KEGG. PCA assessed sample clustering. GEO accession GSE128494.
- qRT-PCR: Conducted on hippocampus, cortex, spleen, small intestine, and hypothalamus (control n=8; RA n=9). Reverse transcription (PrimeScript), detection with SYBR/TB Green, normalized to Gapdh. Targets included Jnk1/2/3, Dusp1, Il1b, Tnf, Ccl5, Cxcl13, Hmgb1, Tlr2, Tlr4.
- ELISA: JNK3 protein in hippocampal extracts quantified with MAPK10 ELISA (control n=5; RA n=6).
- Statistics: Means ± SE; two-group comparisons by Student’s t-test; significance p<0.05 (with trends occasionally reported p<0.10).
- General health: No differences in food intake or body weight between groups. Plasma biochemistry showed no significant differences except a trend to higher creatine kinase in RA group; others unchanged.
- Cognition:
- Y-maze: Total arm entries similar between groups, indicating comparable locomotion. Alternation ratio higher with RA, indicating improved spatial working memory. Reported values: control 54 ± 5.14% vs RA 67.4 ± 2.44% (approaching wild-type ~70%).
- NORT: Discrimination Index (DI) higher in RA vs control at both 5 min and 24 h intervals, indicating improved short- and long-term object recognition memory (e.g., control DI ~0.10 ± 0.13 vs RA ~0.46 ± 0.35).
- Pathology:
- Aβ: IHC showed reduced Aβ accumulation in cortical regions near the amygdala in RA group; quantified plaque area per 1000 μm² significantly lower (n=3/group; p<0.05).
- Phospho-tau (AT8): RA significantly decreased % p-tau-positive cells in hippocampal CA1 vs control (n=3/group; p<0.05); no significant change in DG.
- Hippocampal transcriptomics (microarray): PCA separated RA and control. 549 DEGs (FDR 0.05). GO enrichment included nervous system development, aging, substantia nigra development, long-term potentiation, GABA signaling, circadian regulation, etc. KEGG enrichment included cGMP-PKG, retrograde endocannabinoid signaling, estrogen signaling, glutamatergic/GABAergic synapse, LTP/LTD, TGF-β, and TNF signaling pathways.
- In TNF signaling/JNK axis: Downregulated Map2k1, Jnk3, Atf4, Ccl5; upregulated Dusp1 (JNK phosphatase), suggesting reduced MAPK/JNK signaling.
- JNK pathway modulation:
- qRT-PCR (hippocampus): Jnk3 mRNA decreased; Dusp1 increased. ELISA: JNK3 protein trended lower (p=0.077). In cortex, Jnk1 decreased (p=0.034), Jnk2 and Jnk3 showed trends to decrease (p=0.072 and 0.066).
- IHC: Decreased p-JNK and p-c-Jun positive cells in CA1 with RA, indicating attenuated JNK signaling; reductions co-localized with reduced p-tau.
- Inflammation (central and peripheral): RA reduced expression of inflammatory mediators Il1b, Tnf, Ccl5, Cxcl13, and Hmgb1 in hippocampus, cortex, and spleen; similar reductions seen in intestine for several markers. Tlr2 expression decreased in cortex; Tlr4 decreased in hypothalamus. Collectively indicates systemic and central anti-inflammatory effects, likely contributing to reduced JNK activation.
- Overall: RA supplementation improved cognitive performance, reduced early Aβ and p-tau pathology, particularly in hippocampal CA1, and downregulated hippocampal JNK signaling alongside broad anti-inflammatory effects.
The study addresses whether RA can mitigate tau phosphorylation and cognitive dysfunction in AD beyond its known anti-Aβ activity. RA improved spatial working memory and object recognition in 3×Tg-AD mice without affecting locomotion. Early-stage pathological features—Aβ plaques near the amygdala and p-tau in hippocampus—were reduced by RA, with a prominent decrease in CA1 p-tau, a region crucial for memory and early AD vulnerability. Transcriptomic and molecular analyses converged on suppression of the MAPK/JNK pathway, especially JNK3, coupled with upregulation of Dusp1 and reduced phosphorylation of JNK targets (c-Jun). Given that JNK promotes tau phosphorylation and Aβ production, its downregulation provides a mechanistic link between RA intake and reductions in both tau pathology and Aβ burden. RA also decreased inflammatory mediators centrally and peripherally, consistent with JNK being activated by inflammatory stress; dampening systemic inflammation may reduce central JNK activation and pathology. The findings support JNK3 downregulation in hippocampal pyramidal neurons as a key node through which RA prevents cognitive decline and pathological progression in AD models, highlighting JNK signaling as a therapeutic/preventive target and suggesting diet-derived polyphenols can modulate disease-relevant pathways in vivo.
Dietary rosmarinic acid suppressed AD hallmarks (Aβ plaques and hippocampal p-tau), improved spatial and recognition memory, and attenuated hippocampal JNK signaling—particularly JNK3—in 3×Tg-AD mice. RA also reduced central and peripheral inflammatory mediators, suggesting that systemic anti-inflammatory effects contribute to decreased JNK activation and downstream tau phosphorylation. These results position RA as a promising preventive nutritional component targeting JNK-mediated pathology. Future work should define the temporal sequence between peripheral and central anti-inflammatory effects, clarify RA and metabolite pharmacokinetics and brain penetration, delineate causal links between JNK3 suppression and tau/Aβ changes, and evaluate efficacy across sexes, doses, and disease stages.
- Sample sizes for some assays were modest (e.g., IHC n=3/group; ELISA n=5–6), limiting power and precision.
- Microarray used pooled hippocampal RNA (4 mice/group), which prevents assessment of individual variability.
- Only male mice were studied; sex differences were not evaluated.
- RA was not detected in brain in prior work by the authors, leaving uncertainty about direct central exposure; active metabolites and exact pharmacokinetics remain undefined.
- The temporal order and causality between peripheral anti-inflammatory effects and central JNK suppression were not established.
- Behavioral and pathological assessments focused on early-stage pathology and selected regions; broader brain mapping and longitudinal outcomes were not performed.
- Some molecular changes showed trends rather than statistical significance (e.g., hippocampal JNK3 protein p=0.077; cortical Jnk2/Jnk3).
Related Publications
Explore these studies to deepen your understanding of the subject.