Medicine and Health
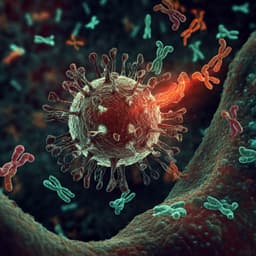
Risk factors for and pregnancy outcomes after SARS-CoV-2 in pregnancy according to disease severity: A nationwide cohort study with validation of the SARS-CoV-2 diagnosis of Nordic Federation of Societies of Obstetrics and Gynecology (NFOG)
A. J. M. Aabakke, T. G. Petersen, et al.
This nationwide cohort study in Denmark explores the critical link between SARS-CoV-2 infection during pregnancy and its impact on maternal health and pregnancy outcomes. The findings reveal heightened risks of hypertensive disorders, early pregnancy loss, preterm delivery, and small-for-gestational-age infants, particularly with hospital admissions amplifying these risks. The research was conducted by a team of experts including Anna J M Aabakke and Tanja G Petersen, among others.
Related Publications
Explore these studies to deepen your understanding of the subject.