Medicine and Health
Nutritional deficiency in an intestine-on-a-chip recapitulates injury hallmarks associated with environmental enteric dysfunction
A. Bein, C. W. Fadel, et al.
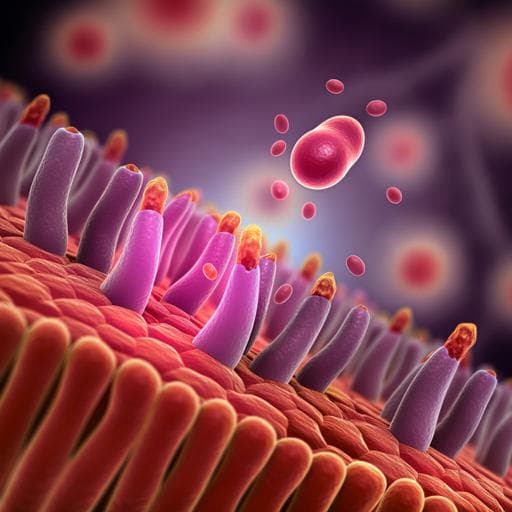
Environmental enteric dysfunction (EED) is a pediatric intestinal disorder associated with chronic inflammation, malnutrition, stunting, cognitive impairment, and poor responses to oral vaccines. Hallmark intestinal features include villous atrophy, nutrient malabsorption, barrier dysfunction, and inflammation. Mechanistic understanding has been limited by the lack of human in vitro models and few animal models, hampering biomarker discovery and therapeutic development. Nutritional deficiencies—particularly tryptophan and niacin (niacinamide)—are implicated in EED pathophysiology and poor growth, yet clinical nutrition interventions have had limited success, likely due to persistent malabsorption and inflammation. The research question asks whether an in vitro human intestine-on-a-chip model, using organoid-derived epithelium from healthy and EED patients, can recapitulate genotypic and phenotypic hallmarks of EED, and to what extent nutritional deficiency versus epithelial-intrinsic factors drive disease features. The purpose is to establish a controllable human EED model to dissect mechanisms (transcriptomic, structural, functional, inflammatory) and to provide a platform for testing candidate nutritional and therapeutic interventions. This is important for understanding and treating a disease affecting millions of children in low- and middle-income countries.
- Model system: Two-channel microfluidic human Small Intestine-on-a-Chip (Emulate S-1) lined with primary intestinal epithelial cells derived from duodenal organoids. Organoids were generated from endoscopic biopsies from pediatric healthy donors (n=3) and EED patients (n=2) who were refractory to nutritional intervention.
- Chip preparation: Chips activated (ER1/2, UV), coated with collagen I (200 µg/ml) and Matrigel (100 µg/ml). Organoid fragments (TrypLE) seeded into the luminal channel; continuous flow 60 µl/h and peristalsis-like strain (10%, 0.15 Hz). After 16–18 days in expansion medium under flow/strain, switched to differentiation medium in the luminal channel for 4 days.
- Nutritional deficiency condition: Dual deficiency medium lacking niacinamide and tryptophan (−N/−T) in both channels prepared by removing these from the DMEM/F12 basal medium and not adding additional niacinamide.
- Experimental groups: Healthy control vs Healthy −N/−T; EED control vs EED −N/−T. Each chip is a biological replicate; multiple donors used for validations as noted in figures.
- Transcriptomics: RNA from chips profiled on Affymetrix Human Clariom D arrays. RMA normalization (oligo:rma). Differential expression with limma; FDR correction (Benjamini–Hochberg). Principal component analysis for uniformity. Comparison to clinical EED signature (SEEM cohort) using Z-score-scaled fold-change and hierarchical clustering. Contextual pathway analysis via COMPBIO NLP platform to identify enriched biological themes and scores (fold enrichment over random clustering).
- Morphology: Differential interference contrast (DIC) imaging (top-down). Confocal immunofluorescence of chip cross-sections: phalloidin (actin), Hoechst (nuclei). Villus-like structure height quantified (membrane to villus tip) across multiple sections/points per chip. Scanning electron microscopy for microvilli integrity (supplementary).
- Mucus layer: Live staining with WGA–Alexa Fluor 488 under flow; longitudinal section imaging and mucus thickness quantification.
- Barrier function: Paracellular permeability (Papp) assessed by apical dosing of Cascade Blue (596 Da) and measuring flux to the basal channel under flow; P = (dQ/dt)/(A·dC).
- Nutrient handling assays: • Fat metabolism: Immunofluorescence for ApoB; fatty acid uptake assay using fluorescent dodecanoic acid measured over time (5–60 min) by widefield fluorescence imaging along the channel. • Amino acid/peptide transport and metabolomics: Lower channel media switched to HBSS, outflows collected over 5 h, frozen, and analysed by LC–MS/MS (Metabolon global platform). Data normalized by total ion count and RMS scaling. Identification of metabolites with differential transport/secretion. Transporter dependency tested using Gly-Sar (1 mM) uptake/transfer with or without PEPT1 inhibitor Gly-Gly (1 mM), quantified by LC–MS/MS.
- Cytokines: Bead-based multiplex ELISA measured nine mediators (IL-6, ICAM-1, VCAM-1, IL-33, MCP-1, MIP-1α, IL-8, Reg3A, IP-10) in luminal and basal channel effluents. Effect of mechanical peristalsis on cytokine secretion evaluated.
- Statistics: Student’s t-test or two-way ANOVA as appropriate; data presented as mean ± s.e.m.; P<0.05 significant. Replicate numbers per figure specified; each chip is one biological replicate.
- Ethics: Healthy biopsies from Boston Children’s Hospital with IRB approval (IRB-P00000529). EED biopsies from The Aga Khan University, Pakistan (ERC 3836-Ped-ERC-15) with informed consent.
- Transcriptomic recapitulation of clinical EED: • EED control vs healthy control chips: 287 differentially expressed genes (DEGs; 86 up, 201 down; q<0.05, FC≥1.5). Shared downregulation of metallothioneins (MT1X, MT1A, MT1F, MT1H, MSMB, MT1M) with clinical EED signature. • Healthy −N/−T vs healthy control: 690 DEGs (556 up, 124 down). Upregulated ATF4 and downstream solute carriers (SLC34A2, SLC7A5, SLC6A9) and LCN2. • EED −N/−T vs EED control: 969 DEGs (522 up, 447 down). Strong overlap and closest clustering with clinical EED signature; 6 of top 10 clinically upregulated genes (60%) also upregulated (e.g., SAA1, SAA2, DUOXA2, DUOX2, CXCL5). • COMPBIO pathway themes in EED −N/−T: Upregulated chemokine signaling (score ~1,834) and amino acid starvation (score ~1,988) with ATF4 upstream; increased tRNA metabolism, DNA damage/p53 methylation, amino acid transporter themes. Downregulated fatty acid uptake (score ~3,591), brush border integrity (score ~3,778), mitosis (score ~3,311), cytochrome P450 (score ~2,582), and fatty acid utilization (score ~2,057).
- Cell-type marker shifts: Enterocyte markers reduced in EED (e.g., MME ↓15-fold, APOB ↓2.7-fold, MTTP ↓2.3-fold); nutritional deficiency further suppressed enterocyte and Paneth cell markers in EED chips, consistent with Paneth cell depletion in EED.
- Structural injury phenotypes under −N/−T: • Villus blunting: Healthy mean height 211 µm (control) vs 60 µm (−N/−T), P<1×10⁻⁶; EED 288 µm vs 48 µm, P=0.000685. • Microvilli loss and disrupted intermicrovillar links observed by SEM. • Mucus thinning: Healthy 448 µm (control) vs 243 µm (−N/−T), P=0.0041; EED 533 µm vs 221 µm, P<1×10⁻⁶. • Barrier compromise: Papp increased 8.9× in healthy (3.82×10⁻⁷ to 3.41×10⁻⁶ cm s⁻¹; P=5×10⁻⁶) and 2.5× in EED (5.71×10⁻⁷ to 1.41×10⁻⁶ cm s⁻¹; P=0.0014) upon −N/−T.
- Impaired nutrient absorption and metabolism: • Fat-related genes down in EED −N/−T: CD36 ↓9.8-fold (q<0.001), APOB ↓10.2-fold (q<0.001), ABCC2 ↓8.2-fold (q<0.001). ApoB protein reduced in EED −N/−T (P=0.012). Fatty acid uptake reduced by ~1.68× (healthy −N/−T) and ~1.69× (EED −N/−T) vs controls. • Amino acid transport/processing down: e.g., SLC36A1 and ANPEP reduced in EED −N/−T; glucose/fructose transporters SLC2A2, SLC2A5 reduced in EED control vs healthy control. • Metabolomics: 36 metabolites showed lower transport in EED vs healthy controls, notably multiple amino acids; 9 overlapped with amino acids reduced in serum of stunted children (e.g., essential: isoleucine, leucine, methionine, phenylalanine, lysine; conditional: arginine, glycine; non-essential: glutamate, serine). Secretion profiles differed: 17 metabolites uniquely secreted by healthy controls; 4 unique to EED controls (xanthine, pyridoxal, α-ketoglutarate, acetylcarnitine). • Transporter dependence: Dipeptide Gly-Sar uptake/transfer reduced by −N/−T and was specifically blocked by PEPT1 inhibitor Gly-Gly, confirming transporter-mediated effects.
- Inflammatory milieu: • −N/−T increased luminal cytokines in healthy chips (IL-6, ICAM-1, VCAM-1, IL-33, MCP-1, MIP-1α, IL-8); Reg3A decreased. EED chips had low baseline cytokines in complete medium but showed significant upregulation under −N/−T. Basal channel also showed higher IL-8, IP-10, MCP-1. Absence of peristalsis reduced IL-8 and MCP-1 secretion.
The intestine-on-a-chip model disentangles environmental (nutritional) and epithelial-intrinsic contributions to EED pathophysiology. Chips lined with EED-derived epithelium reproduced clinical EED transcriptomic signatures only when exposed to niacinamide and tryptophan deficiency, indicating that malnutrition is a key driver of the EED molecular phenotype. In contrast, structural villus atrophy, mucus thinning, barrier dysfunction, and deficits in fatty acid and amino acid handling were induced by −N/−T in both healthy and EED chips, implying these hallmark pathologies can arise from nutritional deficiency alone, independent of preexisting epithelial changes. The data further suggest a feed-forward loop whereby malnutrition diminishes nutrient absorption capacity (downregulating transporters and metabolic pathways) while provoking inflammatory responses that raise energetic demands, exacerbating growth failure. The overlap with clinical cohorts from Pakistan, Zambia, and Bangladesh strengthens the model’s relevance. Functionally, the chip enables simultaneous assessment of barrier integrity, transport, metabolism, and inflammation—outcomes difficult to measure in organoids or in patients—providing mechanistic insight into EED and a platform to test targeted interventions (e.g., restoring ATF4-regulated amino acid metabolism, enhancing brush border integrity, or tailored micronutrient/amino acid supplementation).
This study establishes a human intestine-on-a-chip model that recapitulates key genotypic and phenotypic features of environmental enteric dysfunction, particularly under niacinamide and tryptophan deficiency. Nutritional deficiency is sufficient to induce villus blunting, barrier compromise, and impaired fatty acid and amino acid handling in both healthy and EED epithelium, while EED-specific transcriptomic signatures emerge when EED epithelium is nutritionally stressed. The platform provides a controllable system to dissect mechanisms, identify biomarkers, and evaluate candidate nutritional and pharmacologic therapies. Future work should incorporate immune cells and patient-derived microbiota to model immuno-microbial interactions, expand donor diversity to capture EED heterogeneity, test additional nutrient deficiencies and repletion strategies, and explore personalized nutrition and therapeutic screening leveraging patient biopsies.
- Limited number of EED donors (n=2) and healthy donors (n=3) may constrain generalizability and introduce donor-specific biases.
- Model includes epithelium only; lack of immune, mesenchymal, and neuronal components may underrepresent inflammatory and repair dynamics, though cytokine analyses were performed.
- Nutritional deficiency modeled as dual niacinamide and tryptophan removal; EED in vivo involves broader and variable nutrient deficits and environmental exposures (pathogens, toxins) not simultaneously modeled.
- Microbiome was not included in these experiments; microbial interactions are central in EED pathophysiology.
- Microarray platform (not RNA-seq) was used for chip transcriptomics; although robust, it may offer lower dynamic range and discovery power compared to RNA-seq.
- While peristalsis-like strain and flow were used, in vivo mechanical and hormonal cues are more complex.
Related Publications
Explore these studies to deepen your understanding of the subject.







