Medicine and Health
Neurotoxic amyloidogenic peptides in the proteome of SARS-CoV-2: potential implications for neurological symptoms in COVID-19
M. Charnley, S. Islam, et al.
The study addresses why many COVID-19 patients experience acute and persistent neurological symptoms (e.g., memory loss, sensory confusion, headaches, neuroinflammation, stroke). The authors note increasing evidence of SARS-CoV-2 neuroinvasion and presence of viral proteins in CNS tissues. Because these neurological manifestations resemble features of amyloid-related neurodegenerative diseases (e.g., Alzheimer’s, Parkinson’s), the authors hypothesize that short, amyloidogenic peptides within SARS-CoV-2 proteins might form cytotoxic aggregates that contribute to neurological dysfunction. They focus on accessory open reading frame (ORF) proteins (not essential to viral replication and often intrinsically disordered), proposing that amyloid formation by ORF-derived peptides could serve viral functions (e.g., immune modulation) while inducing host neurotoxicity.
Prior work indicates SARS-CoV-2 can infect multiple neural cell types, with organoid studies suggesting infection/replication in neuronal and retinal cells and persistent virus/neuroinflammation in olfactory tissues. Coronaviruses (including SARS-CoV-1 and SARS-CoV-2) contain sequences with high amyloidogenic propensity, particularly within intrinsically disordered regions of nucleocapsid protein, and amyloid formation can be enhanced by RNA and liquid–liquid phase separation. Amyloids can modulate host responses by acting as inflammatory stimuli, potentially upregulating ACE2 via cytokines, or by interfering with antiviral pathways (e.g., RIPA3 kinase). In inflammatory settings, serum amyloid A can drive systemic AA amyloidosis. Together, these findings suggest potential functional roles for viral amyloids during replication or immune evasion and motivate investigation into SARS-CoV-2 ORF peptides as contributors to COVID-19 neurological symptoms.
- Bioinformatic screening: SARS-CoV-2 ORF6 and ORF10 protein sequences were analyzed with ZIPPER (predicts steric-zipper-forming hexapeptides with Rosetta energies < −23 kcal/mol) and TANGO (aggregation propensity). Multiple highly amyloidogenic windows were identified in ORF6; fewer in ORF10. Based on overlapping high-propensity regions and prior experience with amyloidogenic motifs, two short peptides were selected for synthesis: an ORF6 fragment (ILIIM/ILLIIM) and an ORF10 fragment (RNYIAQVD/RNIAYQD; the selected ORF10 region includes a ZIPPER-predicted NKIVQAC sub-sequence).
- Peptide synthesis and preparation: Peptides (≈95% purity) were obtained commercially. RNYIAQVD was N- and C-capped; IL(I)IIM carried free termini due to synthesis constraints. To maximize monomerization before assembly, lyophilized peptides were dissolved in warmed PBS (90 °C), vortexed, briefly reheated, then slowly cooled to induce self-assembly; parallel assemblies were also performed at 37 °C.
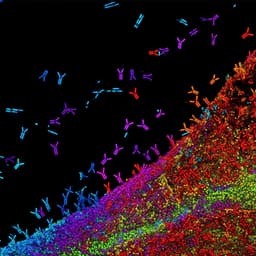
- Biophysical characterization: Atomic force microscopy (AFM; tapping mode on mica) and transmission electron microscopy (TEM) visualized morphology and polymorphism; FiberApp software quantified height and length distributions and persistence length. Small- and wide-angle X-ray scattering (SAXS/WAXS) at the Australian Synchrotron (λ = 1.0323 Å) under flow assessed shape factors and Bragg reflections; circular dichroism (CD; 190–260 nm) with BeStSel deconvolution estimated secondary structure composition and β-sheet twist; Thioflavin T (ThT) fluorescence assays (ex 440 nm/em 482 nm) monitored assembly kinetics; amyloid-binding dyes/antibodies and fluorescence microscopy assessed amyloid-specific staining.
- Molecular modeling: Atomistic models of 2D sheet-like amyloid assemblies were constructed and simulated (periodic boundaries, implicit/explicit solvent as described) to reproduce WAXS peak positions and infer steric-zipper interfaces and sheet stacking consistent with SAXS/WAXS.
- Cell assays: Human neuroblastoma SH-SY5Y cells were cultured in DMEM-F12 with FCS and antibiotics. Cytotoxicity was measured by MTT after 48 h exposure to a concentration series. Flow cytometry (Annexin V/7-AAD) quantified viable, early apoptotic, necrotic, and late apoptotic cells. Manual cell counts with trypan blue assessed overall cell number after 48 h. Statistical analyses used one-way ANOVA with Tukey post hoc tests (n ≥ 3).
- Identification of amyloidogenic peptides: Bioinformatic tools (ZIPPER, TANGO) highlighted multiple high-propensity regions in ORF6 and a key region in ORF10; peptides from ORF6 (ILIIM/ILLIIM) and ORF10 (RNYIAQVD/RNIAYQD) were selected and synthesized.
- Rapid self-assembly and polymorphism: Both peptides self-assembled rapidly at 37 °C into polymorphic nanostructures. AFM/TEM revealed predominately needle-like crystalline structures and twisted fibrils; both peptides formed multi-laminar stacks. ILIIM formed wider, laterally associated crystals (2–3 μm wide), whereas the ORF10 peptide formed longer, thinner, needle-like assemblies with less lateral association. Step heights suggested multilayer stacking with heterogeneous thickness.
- Quantitative morphology: Persistence length analysis indicated very straight fibrils for both, with the ORF10 peptide showing greater stiffness (λ ≈ 412.9 nm) than ILIIM (λ ≈ 32.0 nm). Length distributions were biphasic; ORF10 peptide favored longer, thinner assemblies, while ILIIM favored wider, shorter assemblies.
- SAXS/WAXS and CD confirm amyloid structure: SAXS showed a q⁻² dependence for ILIIM (consistent with 2D sheet-like structures) and a q⁻⁴ dependence for the ORF10 peptide (sharp-surfaced aggregates). WAXS displayed a strong Bragg peak at q ≈ 1.38 Å⁻¹ (d ≈ 4.6 Å) for both, characteristic of β-sheet spacing; ILIIM additionally showed a Bragg reflection at q ≈ 0.858 Å⁻¹ (d ≈ 11 Å), consistent with a hydrophobic steric-zipper intersheet spacing. CD spectra indicated β-sheet-rich assemblies; BeStSel analysis suggested ILIIM β-sheets with left-handed twist at higher concentration and mixed twists at lower concentration, and predominantly right-handed β-sheets for the ORF10 peptide.
- Modeling supports 2D sheet-like assemblies: Atomistic models of ILIIM formed parallel β-sheets with hydrophobic steric-zipper interfaces; simulated scattering reproduced main WAXS features and was consistent with 2D sheets that could laterally stack into multilaminar crystals.
- ThT kinetics: Both peptides exhibited rapid amyloid formation with minimal or no lag phase, reaching plateau within hours; ThT signal intensity increased with concentration, and the ORF10 peptide showed strong concentration dependence.
- Co-assembly: Mixed peptides co-crystallized into highly ordered, interlocking 2D crystals not observed in single-peptide assemblies, indicating potential cross-assembly.
- Cytotoxicity to neuronal cells: Both peptide assemblies were highly toxic to SH-SY5Y neuroblastoma cells after 48 h. Viability dropped below 50% at concentrations as low as ~0.04 mg/mL (ILIIM) and as low as ~0.04–0.32 mg/mL for the ORF10 peptide depending on assay/condition. Flow cytometry showed a 3–5-fold increase in late-stage apoptosis on average versus control, with a pronounced increase for the ORF10 peptide at 2.5 mg/mL (reported up to hundreds-fold); necrosis did not increase, implicating apoptosis as the primary death pathway. Significant reductions in cell counts were observed at ≥0.04 mg/mL (ILIIM) and ≥0.32 mg/mL (ORF10 peptide).
- Morphology–toxicity relationship: Laterally associated, wider crystalline assemblies (ILIIM) correlated with higher toxicity and apoptosis at lower thresholds compared to the longer, thinner fibrils of the ORF10 peptide, suggesting amyloid polymorphism modulates cytotoxicity.
The findings support the hypothesis that short, amyloidogenic sequences within SARS-CoV-2 ORF proteins can form β-sheet-rich amyloid assemblies that are directly neurotoxic, primarily by inducing apoptosis in neuronal cells. The structural data (AFM/TEM, SAXS/WAXS, CD) confirm robust amyloid formation with distinct polymorphisms: ILIIM forms 2D sheet-like crystals that laterally associate, while the ORF10 peptide forms thinner, longer fibrils. Modeling indicates hydrophobic steric-zipper interfaces consistent with the observed WAXS peaks. These structural polymorphisms correlate with cytotoxic profiles, with ILIIM’s wider, crystalline assemblies showing higher toxicity at lower concentration thresholds. The results align with literature indicating that viral proteins can harbor amyloidogenic regions and that amyloids can act as inflammatory stimuli or modulate host antiviral responses. Given reported neuroinvasion and persistent neurological symptoms in COVID-19, the demonstrated neurotoxicity of ORF-derived amyloid assemblies provides a plausible molecular mechanism contributing to COVID-19 neuropathology and possibly long-COVID symptoms. The data also suggest that the highly cytotoxic nature of ORF6 observed elsewhere may be linked to its intrinsic amyloidogenicity.
This study identifies two short peptides within SARS-CoV-2 ORF proteins (ORF6 and ORF10) that rapidly self-assemble into β-sheet-rich amyloid structures exhibiting pronounced polymorphism and strong neurotoxicity toward human SH-SY5Y cells via apoptosis. Multimodal biophysical characterization and molecular modeling corroborate amyloid architecture, including steric-zipper interfaces and multilaminar sheet stacking. The results support a potential amyloid etiology for some neurological symptoms of COVID-19 and implicate ORF-derived amyloid assemblies as candidate molecular drivers of neurotoxicity. Future work should: (i) validate amyloid formation and neurotoxicity in vivo and in primary neuronal models; (ii) investigate full-length ORF proteins and other SARS-CoV-2 proteins for amyloidogenic behavior; (iii) quantify expression/localization of these proteins/peptides in infected tissues; (iv) determine mechanisms of neuronal membrane interaction and apoptotic signaling; (v) assess the biological relevance of co-assembly; and (vi) examine patient samples for amyloid signatures attributable to viral proteins.
- In vitro peptide fragments: The study uses short peptide fragments rather than full-length viral proteins; in vivo processing, post-translational modifications, and cellular environments may alter aggregation and toxicity.
- Cell line model: Neurotoxicity was assessed in SH-SY5Y cells; primary neurons or in vivo models are needed to generalize to human CNS pathology.
- Physiological relevance of concentrations: Effective toxic concentrations in vitro may differ from peptide/protein concentrations achievable in infected tissues.
- Expression uncertainty: ORF10 is reported to have low expression and uncertain functional importance; the in vivo abundance of the studied fragments is unknown.
- Structural heterogeneity: While SAXS/WAXS/CD support amyloid structure, definitive atomic-resolution structures in solution were not obtained; polymorphism complicates precise structure–function mapping.
- Co-assembly significance: The biological relevance of mixed-peptide co-crystallization remains untested.
- Peptide capping: Only the ORF10 peptide was capped; terminal charges on the ORF6 peptide may influence assembly and toxicity compared to native contexts.
Related Publications
Explore these studies to deepen your understanding of the subject.