Medicine and Health
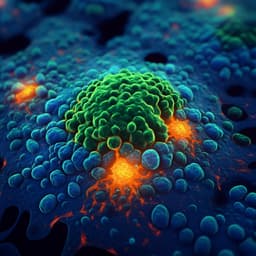
Neoantigen-specific CD8 T cells with high structural avidity preferentially reside in and eliminate tumors
J. Schmidt, J. Chiffelle, et al.
This groundbreaking research by Julien Schmidt, Johanna Chiffelle, Marta A. S. Perez, and colleagues explores the relationship between T cell antigen recognition strength and cancer immunotherapy effectiveness. By analyzing 371 CD8 T cell clones, the study reveals that T cells from tumors have higher functional and structural avidity compared to those from blood, highlighting neoantigens as a key player in tumor infiltration. These findings pave the way for identifying potent T cells for personalized cancer treatments.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.