Engineering and Technology
Multiscale architecture design of 3D printed biodegradable Zn-based porous scaffolds for immunomodulatory osteogenesis
S. Li, H. Yang, et al.
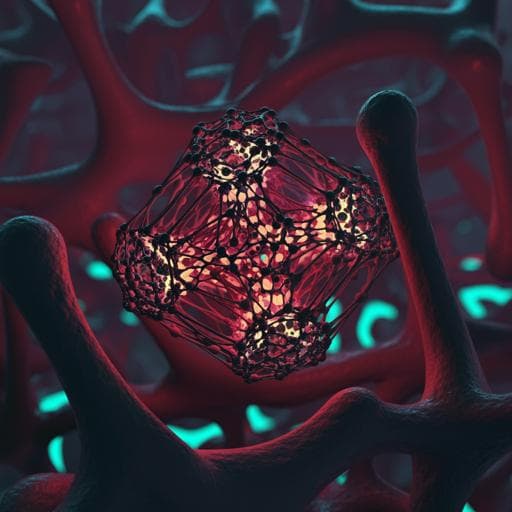
Metallic zinc (Zn) has unique electrochemical and structural properties and is abundant in humans, functioning as a cofactor in a large portion of the proteome. The emergence of Zn-based biomaterials has opened avenues in orthopedics for biodegradable implants with mechanical strength and bioactivity. However, a mismatch exists between slow degradation of bulk Zn-based implants (potentially requiring a decade) and the 3–6 month bone repair cycle. Recent advances in 3D printing of biodegradable Zn alloys aim to reduce material usage and tune structural properties, but increased porosity and surface area raise risks of overdose Zn toxicity due to accelerated degradation. The immune response plays a central role in tissue repair, and osteoimmunomodulation—modulating immune cell behavior, particularly macrophages—can improve outcomes. Macrophages regulate inflammation, angiogenesis, and osteoblast activity; their polarization (M1/M2) is influenced by ion release, surface topography, and pore geometry at multiple scales. Zn2+ transport and homeostasis affect macrophage fate; nanoscale surface cues can modulate macrophage filopodia and polarization; and pore geometry affects cell organization and degradation behavior. Therefore, multiscale architecture design (composition, surface, and geometry) may orchestrate immune responses and bone regeneration. Here, Zn-based alloy scaffolds with up to 90% porosity were fabricated. A high-strength Zn-Li alloy system (notably 0.8 wt% Li) was selected to mitigate Zn overdose via co-release of Zn and Li. Surface treatments (ultrasound, acid etching, electrochemical polishing) created nanoscale patterns. Gyroid (G) minimal surface units were compared with body-centered cubic (BCC) lattices to study structure–degradation–regeneration relationships emphasizing osteoimmunomodulation across genes, cells, and tissues.
The paper reviews prior findings that bulk Zn-based implants degrade too slowly for typical bone healing timelines, motivating porous, 3D-printed designs. It discusses how increased porosity enhances degradation and potential Zn toxicity, highlighting the need to understand structure–degradation–function relationships. The osteoimmune paradigm is emphasized: biomaterials that modulate macrophage behavior can promote bone regeneration. Prior works show nanoscale topographies (e.g., 90 nm TiO2 honeycombs) induce macrophage filopodia via RhoA/ROCK signaling and modulate cytokine secretion; pore geometry influences multicellular organization and degradation; Zn ions can dose-dependently shift macrophages toward M2 phenotypes; Li can enhance anti-inflammatory cytokines and osteogenesis. Degradation of Zn scaffolds scales positively with porosity and inversely with pore size. These insights underpin the multiscale design approach (composition Zn-Li, surface nano-roughness, gyroid geometry) to balance degradation with immunomodulation and osteogenesis.
Materials and alloy preparation: Zn-Li alloys were prepared from pure Zn (99.995 wt%) and a Zn-Li master alloy (Hunan Rare Earth Metal Material Research Institute). As-cast alloys were hot-extruded into 10 mm rods at 210 °C (extrusion ratio 16:1). Pre-alloyed Zn-0.8Li rods were gas-atomized (argon) to powders (D50=29.7 µm). Powder composition was verified by ICP-OES (Li content 0.69 ± 0.01 wt%). 3D printing (L-PBF): Powders were dried (vacuum oven, 70 °C, 4 h). Printing used a commercial L-PBF system (BLT) with Yb fiber laser (IPG YLR-500, 1070 nm, 70 µm spot). Argon chamber (>99.99% purity, O2<120 ppm). Substrate: 20 mm pure Zn plate, ground and ethanol-cleaned. Optimized parameters for Zn-0.8Li: laser power 40 W, scan speed 800 mm/s, hatch spacing 70 µm, layer thickness 20 µm; zig-zag infill with 67° rotation per layer and contouring. Gyroid (G) and BCC structures printed in sizes: Ø10×2 mm (cell and electrochemistry), Ø6×6 mm (mechanical and immersion tests), Ø3×4 mm (animal implants). Surface treatments and characterization: As-printed scaffolds were ultrasonically cleaned in ethanol for 24 h. Acid etching: 10% acid solution for 10–60 s. Electrochemical (EC) polishing: phosphoric acid/ethanol electrolyte at 1 A, 60–120 s, 55 °C bath. Surface morphology assessed by SEM; roughness by AFM (tapping mode, 0.5 Hz). Microstructure characterized by SEM (etched 4% HNO3/alcohol, 5–10 s), XRD (10–90°, 2°/min, step 0.02°), and TEM (samples thinned to 60 µm, 3 mm disks, ion milling; STEM HAADF at 300 kV). Mechanical testing: Tensile specimens from extruded rods per ASTM E08-04a (Instron 5969, 1×10⁻³ s⁻¹). Compressive tests on Zn-0.8Li scaffolds (G and BCC) at 3×10⁻³ s⁻¹; yield strength from 0.2% offset; post-deformation SEM. Electrochemical and degradation tests: Three-electrode cell (Pt counter, saturated calomel reference, sample as working) in HANKS’ solution at 37 °C. Immersion for 23 h, then OCP (1 h). EIS (10 mV perturbation, 10–10⁻² Hz). SVET measured potential and pH distributions after 24 h immersion (HANKS’, 100 µm step). XPS (NAP-XPS) identified corrosion products after immersion. Dynamic immersion: continuous perfusion system (500 mL HANKS’, peristaltic pump 10 rpm, 37 °C) for 28 days with solution renewal every 2 days; SEM and Micro-CT (Zeiss Xradia 520 Versa, 120 kV, 66.7 µA) analyses; 3D reconstructions (CTvox 3.0). Weight loss measured after removing corrosion products (0.1 M HCl). Diffusion measurements: Two-compartment setup (donor ZnCl2 solution, receiver DI water) with scaffold centrally mounted; pre-wetting 2 h; stirring and 37 °C. Periodic sampling (0.5 mL) and ICP quantification of Zn. Flux, permeability, and diffusion coefficients calculated (partition coefficient K≈1). Cell culture and cytocompatibility: RAW264.7 (DMEM +10% FBS) and MC3T3-E1 (MEM-α +10% FBS) cultured at 37 °C, 5% CO2. Direct seeding on scaffolds (10×2 mm) with 1×10⁶ cells per sample for 2 h, then 2 mL medium. Live/dead staining after 48 h (EthD-1 and Calcein AM), imaging by fluorescence microscopy; quantification of viable cells per unit and per area using Image Pro Plus. Cytoskeleton staining (DAPI, phalloidin TRITC or FITC) and confocal imaging; SEM of adhered cells after fixation and graded ethanol dehydration. Extract preparation and macrophage assays: Alloy extracts prepared following ISO 10993-12 (UV sterilization; medium at 1.25 mL/cm², 37 °C, 24 h); ICP for ion concentrations. RAW264.7 cultured with 5-fold diluted extracts for 48 h. Macrophage polarization assessed by immunofluorescence (iNOS, CD206) and qRT-PCR (M1: iNos, Il-1β, Tnf-α; M2: Il-4, Il-10, Arg1). Transcriptomics: RAW264.7 treated with 5-fold G scaffold extracts vs. control; RNA-seq, differential expression, GO and KEGG analyses (bioinformatics.com.cn); significance thresholds padj ≤ 0.05 and |log2FC| ≥ 1. Osteogenic conditioning: Conditioned medium (CM) prepared from RAW264.7 supernatants after 48 h treatment with BCC or G extracts, centrifuged, 0.22 µm filtered, stored −80 °C; mixed 1:2 with fresh MEM-α. MC3T3-E1 cultured in CM with osteogenic supplements (10 mM β-glycerophosphate, 0.25 mM ascorbic acid). ALP staining and activity at 7 days; ARS staining at 14 days. qRT-PCR for osteogenic genes (Alp, Opg, Opn, Col1a1) at 7 days; IF for RUNX2 and OSX. In vivo studies: Ethical approval NRIFH 21-2203-18; rat femoral condyle defect model (Sprague-Dawley, 12-week-old males, 350–400 g). Cylindrical defects (3×4 mm) created in femoral condyle; implantation of BCC or G scaffolds (3×4 mm); euthanasia at 3 days, 1 month, 3 months. Sample processing: non-decalcified (MMA embedding, sectioning to 50 µm) and decalcified (EDTA 6–8 weeks, paraffin, 5 µm sections). Imaging: SEM of polished MMA sections; XRF mapping (Bruker M4 Tornado, 50 kV, 600 µA, filtered, vacuum 20 mbar, 20 µm step, 5 ms/pixel); methylene blue acid fuchsin staining; SHG imaging (860 nm excitation, detect 420–430 nm). Histology/IHC: iNOS, CD163, OCN, ALP staining; quantification of IOD/area. Micro-CT (Skyscan1176, 18 µm resolution, 40 kV, 250 µA); reconstruction and morphometry (BV/TV, Tb.Sp, bone ingrowth ratio, pore size). Statistics: one-way ANOVA with Tukey post hoc; box-whisker plots as described; p<0.05 considered significant.
- Composition and microstructure: Zn-0.8Li alloy exhibits a lamellar eutectoid microstructure (LiZn4 and Zn phases) with 200–300 nm interlamellar spacing. Mechanical trade-off across Li contents identifies Zn-0.8Li as optimal for strength–ductility balance. Electrochemical impedance increases with Li content; after 24 h in SBF, corrosion products include ZnO and Li2CO3. Surface potential uniform in Zn-0.2Li and Zn-0.8Li, but Zn-0.8Li surface pH is higher (9.2–9.3 vs 7.5–7.6 for Zn-0.2Li). Extracts from Zn-0.8Li show Zn:Li ≈ 4:1 (Zn 17.1 µg/mL; Li 3.9 µg/mL). Macrophages exposed to Zn-Li extracts, especially Zn-0.8Li, show increased CD206 and decreased iNOS, with upregulated Il-4, Il-10, Arg1 and downregulated Tnf-α, iNos, Il-1β.
- Surface morphology: EC polishing removes unmelted powders and creates wavy protrusions with higher roughness (Ra=114 nm) than acid-etched surfaces (Ra=79 nm). RAW264.7 cells display enhanced adhesion, filopodia anchoring, and increased spread area on EC-polished surfaces; ultrasound/acid-etched surfaces show clustered, round cells with poor adhesion. Acid etching reduces impedance (activates surface), while EC polishing partially repassivates.
- Mechanical properties of scaffolds: Porosity 86–90% with ~10× specific surface area vs bulk. Bulk Zn-Li compressive yield stress is ~391.74 MPa; adding 80% porosity reduces strength by ~97%. G-unit scaffolds show higher strength and similar modulus compared to BCC. BCC peaks at ~−2% strain then collapses (~10% strain) with joint cracking; G shows a stable plateau and resists crack propagation (cracks appear near 40% strain) with uniform deformation.
- Corrosion behavior: In PDP, G shows passivation at overpotential <0.2 V, BCC shows active dissolution. BCC corrosion is non-uniform with deep pits at connections; G exhibits small, shallow, homogeneous pits. EIS indicates higher charge transfer resistance in G; low-frequency response suggests stronger mass transfer effects in BCC. In 28-day dynamic perfusion, BCC accumulates corrosion products sealing pores and exhibits severe strut corrosion; G accumulates less product and retains intact struts. BCC weight loss is ~2× G, and BCC loses ~90% compressive strength while G maintains ~40% mechanical integrity after 28 days. Diffusion tests show Zn ion diffusion becomes more anisotropic in BCC than G over time.
- In vitro biocompatibility: Majority of RAW264.7 and MC3T3-E1 cells remain viable after 48 h on both scaffolds. RAW264.7 adhesion is ~3-fold higher on G than BCC; RAW264.7 on G exhibit extensive, radially extended F-actin filopodia and elongated morphology. MC3T3-E1 adheres and spreads on both; cell numbers slightly higher on G without significant density difference per area.
- Macrophage polarization and osteoinduction in vitro: Macrophages in scaffold extracts (48 h) transition to elongated M2-like morphology, with lower nucleus-to-cytoskeleton area ratio in G group. Both BCC and G upregulate CD206 and suppress iNOS; G yields lowest Tnf-α and highest Il-4, Il-10, Arg1. RNA-seq (G vs control) shows 287 up- and 58 down-regulated genes; GO enrichment in proliferation, adhesion, cytoskeleton, and immune response; KEGG shows downregulated MAPK and upregulated JAK/STAT pathways, consistent with M2 polarization. MC3T3-E1 in macrophage-conditioned media show higher ALP staining/activity at 7 days and more ARS-positive mineralization at 14 days for G vs BCC; osteogenic genes (Alp, Opg, Opn, Col1a1) are highest in G; RUNX2/OSX IF supports enhanced osteogenic differentiation in G.
- In vivo degradation: At 3 days, intact struts are visible; XRF detects Zn spread in pores/edges indicating early degradation. At 1 month, BCC shows severe, non-uniform degradation with pores filled by products; G degrades uniformly with Ca signals in pores indicating mineralization. At 3 months, BCC exhibits collapse with heterogeneous degradation; G retains metallic structure with extensive new bone ingrowth in interconnected pores.
- In vivo immune response and early osteogenesis: At 3 days, M1 (iNOS+) predominates; at 1 month, inflammation resolves. G shows fewer iNOS+ cells and more CD163+ (M2) cells at both time points; M2/M1 ratio consistently higher in G. ALP and OCN staining at 1 month are significantly higher around G than BCC, indicating more active osteogenesis.
- Bone regeneration (3 months): Micro-CT and histology show G pores filled with new bone; BCC shows less hard tissue and more degradation products. Quantitatively, BV/TV is significantly higher and Tb.Sp significantly lower in G vs BCC. Bone-ingrowth-favorable pore sizes are 200–600 µm. SHG imaging shows well-aligned type I collagen fibers oriented along G struts at 3 months; BCC exhibits point-like, poorly oriented collagen.
- Mechanistic summary: Multiscale design (Zn-0.8Li composition, EC-polished nanoscale roughness, G minimal surface geometry) tempers degradation rate, promotes uniform corrosion, enhances M2 polarization via JAK/STAT (upregulating IL-4/IL-10), and accelerates osteogenesis and collagen organization.
The study addresses the central challenge of balancing rapid scaffold degradation with avoidance of Zn overdose toxicity when moving from bulk to highly porous implants. By alloying Zn with 0.8 wt% Li, the microstructure (lamellar LiZn4/Zn) modifies local corrosion chemistry, elevates pH, forms Li2CO3 and ZnO, and shifts ion release toward a Zn:Li ratio of ~4:1, which in turn augments macrophage M2 polarization and anti-inflammatory cytokines while suppressing M1 markers. Mesoscale EC-polished nano-rough surfaces enhance early macrophage adhesion, spreading, and filopodia, suggesting rapid functional activation that can steer a favorable immune microenvironment. At the macroscale, gyroid architecture yields higher mechanical robustness and notably more uniform, slower degradation than BCC, maintaining structural integrity and open porosity for tissue ingrowth. These effects collectively promote an early switch from M1 to M2 at the implant interface, increase early osteogenic markers (ALP, OCN), and result in superior bone volume, reduced trabecular separation, and aligned type I collagen deposition at 3 months. Transcriptomics corroborate downregulated MAPK (M1-associated) and upregulated JAK/STAT (M2-associated) pathways in macrophages exposed to G-scaffold extracts, consistent with the observed immunomodulatory osteogenesis. Overall, a multiscale design strategy orchestrates immune responses and degradation kinetics to enhance bone regeneration in load-bearing contexts.
This work demonstrates a multiscale architecture strategy for 3D-printed Zn-based porous scaffolds that integrates: (1) Zn-0.8Li alloy composition to optimize strength and modulate corrosion/ion release favoring M2 macrophage polarization; (2) EC-polished nanoscale wavy surface patterns to enhance macrophage adhesion and functionalization; and (3) gyroid minimal surface geometry to achieve uniform, appropriate degradation and mechanical stability. The approach promotes early anti-inflammatory immune responses, upregulates osteogenic markers, aligns collagen deposition, and enhances new bone formation. These findings suggest strong potential for Zn-Li gyroid scaffolds in load-bearing bone defect repair. Future studies may explore longer-term in vivo performance, optimization of alloying/surface parameters, and translation to larger animal models and clinical scenarios.
Related Publications
Explore these studies to deepen your understanding of the subject.