Medicine and Health
Multi-biofunctional graphene oxide-enhanced poly-L-lactic acid composite nanofiber scaffolds for ovarian function recovery of transplanted-tissue
L. Yan, L. Wang, et al.
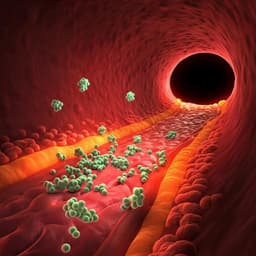
Cancer therapies can irreversibly damage ovarian function, threatening fertility in girls and young women. Ovarian tissue cryopreservation and transplantation (OTC/OTT) enable fertility preservation, but grafts suffer ischemia-reperfusion injury and follicle loss before revascularization. Whole-ovary transplantation with vascular anastomosis is complex, and while co-transplanting exogenous endothelial cells may help perfusion, biomaterial-assisted strategies remain underexplored. Graphene oxide (GO) features a large surface area and oxygen-containing functional groups that can promote cellular interactions and angiogenesis. Poly-L-lactic acid (PLLA) is biocompatible and degradable but has low initial strength and fast strength decay. The research question is whether incorporating GO into PLLA to form electrospun composite nanofiber scaffolds can enhance mechanical properties, promote angiogenesis, and improve fusion and survival of transplanted ovarian tissue to restore ovarian function in a POI mouse model.
- OTC/OTT has led to >130 births by 2017, yet ischemia after transplantation reduces primordial follicles and limits outcomes.
- Whole-ovary transplantation with arteriovenous anastomosis shortens ischemia but is clinically challenging (cryoprotectants, surgical complexity).
- Co-transplantation with engineered endothelial cells can accelerate perfusion; however, a biomaterial co-transplantation system had not been reported.
- GO is amphiphilic with epoxy, hydroxyl, and carboxyl groups, promoting cell proliferation, differentiation, and angiogenesis; it can enhance polymer mechanics and interface interactions.
- PLLA is widely used clinically, offering biocompatibility and degradability, but requires mechanical enhancement for supporting tissue fusion and regeneration.
- Prior studies showed GO’s angiogenic properties and potential to modulate eNOS/NO signaling, but in vivo application to improve organ transplantation had not been demonstrated.
- Materials: Graphite, DCM, DMF (Alfa Aesar); PLLA (Mn ≈ 300,000; Jinan Daigang); other analytical-grade reagents; DI water.
- Animals: Female C57BL/6 mice (8 weeks, 19–21 g) under standard conditions; procedures approved by institutional animal care.
- GO synthesis: Modified Hummers’ method with KMnO4 in H2SO4, quenching with H2O2, washing (HCl), dialysis (3,000 Da cutoff), sonication, and freeze-drying.
- GO/PLLA dispersions: PLLA 10 wt% dissolved in DCM/DMF (1:1 v/v) 12 h; GO (10 mg/mL) dispersed by ultrasonication; GO suspensions (0.5, 1.0, 4.0 wt% relative to PLLA) added and stirred 12 h; bath sonication and overnight standing before use.
- Electrospinning: 15 kV, feed 0.30 mm/min via 27 G needle, 20 cm tip-to-collector distance, drum at 120×g, 25 °C, ~50% RH; samples freeze-dried 48 h and cut to uniform size.
- Physical characterization: SEM (Hitachi S-4800), AFM (Bruker Multimode 8), XPS (ESCALab220i-XL), Raman (Renishaw inVia, 514 nm), water contact angle (Krüss DSA 100), porosity (segmental method), mechanical testing (Zwick 1435).
- In vitro cytotoxicity: Granulosa cells (GCs) cultured in DMEM + 10% FBS; CCK-8 viability after 24 h exposure to GO (0–100 µg/mL); Live/Dead staining (Calcein AM/PI) for GO (0–100 µg/mL) after 24 h.
- In vitro degradation: Square scaffolds (10×10 mm) immersed in DI water, PBS (pH 7.4), DMEM, or DMEM+10% FBS at 37 °C with shaking; timepoints 3, 7, 14, 21, 28 days; SEM and Raman; weight loss quantified.
- Isolation/culture of GCs: From ovaries of 8-week C57BL/6; identified by FSHR; seeded on plates and GO/PLLA scaffolds.
- POI model: Cisplatin 1.5 mg/kg i.p. daily for 10 days; controls received saline. Body weight, ovarian histology, and serum hormones (E2, AMH, FSH, LH) assessed.
- Ovarian tissue transplantation: In POI recipients, unilateral half-ovary removed; donor normal ovarian cortical blocks loaded on GO/PLLA scaffolds (0.0 or 1.0 wt% GO) or without scaffold transplanted orthotopically into the ovarian cyst; harvested at 1, 2, 3 months.
- Oocyte collection and IVM: After PMSG (10 IU) 46–48 h, GV oocytes collected; cultured in α-MEM with FSH, FBS, EGF; PB1 extrusion assessed after 16–18 h.
- Histology and immunohistochemistry: H&E for follicle staging/count; IHC for CD31, CD34, FSHR; MVD quantified per 200× field.
- TUNEL assay: One-step TUNEL on 4-µm sections with positive/negative controls; DAPI counterstain.
- Hormone assays: Serum E2, AMH, FSH, LH via ELISA (Cloud-Clone) at 1, 2, 3 months post-transplant.
- Western blot: eNOS, p-eNOS, GAPDH; densitometry with Quantity One; NO in GCs supernatant quantified with NO detection kit after co-culture with scaffolds of varying GO content.
- Statistics: Data as mean±SD; one-/two-way ANOVA, Student’s t test, chi-square; significance at P<0.05.
- Scaffold fabrication and properties:
- GO nanosheets exfoliated (~1 nm); when mixed with PLLA, thickness ~2 nm with increased surface roughness, indicating PLLA adsorption on GO.
- Electrospun GO/PLLA scaffolds formed continuous, uniform nanofibers; no GO protrusion; average fiber diameter decreased with increasing GO.
- Water contact angle decreased from 66.7° (0 wt% GO) to 55.6° (4 wt% GO), indicating increased hydrophilicity; porosity high (0.81–0.84).
- Mechanical performance improved at 1.0 wt% GO (Young’s modulus 1.09 GPa; strength 1.67 MPa), exceeding pure PLLA; slight decrease at 4.0 wt% GO likely due to GO aggregation.
- Degradation: In DMEM, PLLA weight loss at 28 days was 7.06% (DMEM) and 9.77% (DMEM/FBS); GO reduced degradation rate and maintained morphology longer in vitro and in vivo.
- Cytotoxicity and in vitro cell response:
- GO nanosheets showed minimal cytotoxicity to GCs across tested concentrations.
- GCs on 1.0 wt% GO/PLLA displayed the lowest dead-cell percentage and significantly higher proliferation (EdU+) than 0.0, 0.5, and 4.0 wt% groups.
- POI model: Cisplatin induced ovarian atrophy, decreased E2 and AMH, and increased FSH and LH, confirming POI.
- In vivo transplantation outcomes (POI mice):
- Transplanted ovary survival rate: Ovary+1.0 wt% GO/PLLA 86.7% (n=15) vs Ovary+0.0 wt% GO/PLLA 53.8% (n=13) vs Ovary alone 28.6% (n=14).
- Visible angiogenesis and follicles on graft surface most evident with 1.0 wt% GO/PLLA.
- Oocyte IVM PB1 extrusion: Normal 83.3%; Ovary alone 0.0%; Ovary+0.0 wt% GO/PLLA 50.0%; Ovary+1.0 wt% GO/PLLA 85.7%.
- TUNEL: Lower apoptosis (weaker TUNEL IntDen) in Ovary+1.0 wt% GO/PLLA vs Ovary and Ovary+0.0 wt% GO/PLLA; comparable to negative control.
- Serum hormones:
- 1 month: E2 (pg/mL) 28.50±5.07 (1.0 wt%) vs 18.76±2.14 (Ovary) vs 19.38±3.44 (0.0 wt%); FSH and AMH not significantly different.
- 2 months: E2 41.27±3.32 (1.0 wt%) vs 20.18±2.18 (Ovary); AMH higher and FSH lower in 1.0 wt% vs Ovary and 0.0 wt%.
- 3 months: E2 46.44±5.28 (1.0 wt%) vs 20.76±3.70 (Ovary); AMH (ng/mL) 2.30±0.38 (1.0 wt%) vs 0.82±0.17 (Ovary) and 0.98±0.23 (0.0 wt%); FSH (ng/mL) 21.50±2.05 (1.0 wt%) vs 41.84±3.54 (Ovary) and 37.15±2.46 (0.0 wt%).
- Follicles: Total follicles increased by 2–3 months in scaffold groups; at 3 months, Ovary+1.0 wt% GO/PLLA had significantly more follicles than 0.0 wt% and Ovary; contralateral ovaries showed few follicles with no significant group differences.
- Angiogenesis:
- Higher CD31 and CD34 expression and MVD (per 200× field) in transplanted ovaries with 1.0 wt% GO/PLLA > 0.0 wt% > Ovary alone; no significant differences in contralateral side.
- On scaffolds in vivo, FSHR-positive GCs were present; CD31/CD34 expression higher on 1.0 wt% GO/PLLA than 0.0 wt%.
- Mechanism:
- p-eNOS levels in transplanted ovarian tissue increased in both 0.0 wt% and 1.0 wt% scaffold groups vs Ovary alone; total eNOS unchanged.
- NO production in GCs supernatant increased with scaffolds (0.0, 0.5, 1.0, 4.0 wt%), with the most pronounced rise at 1.0 wt%, consistent with p-eNOS trends, implicating eNOS/NO signaling in angiogenesis and graft survival.
Incorporating GO into PLLA produced electrospun nanofiber scaffolds with enhanced mechanical integrity, increased hydrophilicity, and a porous network favorable for cell infiltration. These properties, together with GO’s bioactivity, supported better graft-host fusion and angiogenesis in vivo. In a cisplatin-induced POI mouse model, co-transplantation of ovarian cortex with 1.0 wt% GO/PLLA scaffolds significantly improved graft survival, follicle development, and endocrine recovery (higher E2 and AMH, lower FSH) compared with transplantation alone or PLLA-only scaffolds. Enhanced CD31/CD34-positive microvessel density in grafts and on scaffolds indicated robust neovascularization. Elevated p-eNOS (with unchanged total eNOS) and increased NO production suggest activation of eNOS/NO signaling as a mechanism contributing to angiogenesis and tissue survival. The 1.0 wt% GO loading emerged as an optimal balance between mechanical reinforcement, degradation control, and pro-angiogenic cellular response, whereas higher GO (4.0 wt%) risked aggregation and diminished mechanical gains. Overall, the findings demonstrate that GO/PLLA scaffolds directly address ischemia-related follicle loss by accelerating revascularization, thereby restoring ovarian function after transplantation.
The study establishes GO/PLLA electrospun nanofiber scaffolds as a multi-functional biomaterial that enhances mechanical performance, modulates degradation, promotes angiogenesis, and improves survival and function of transplanted ovarian tissue in a POI mouse model. An optimal 1.0 wt% GO content yielded the best outcomes in graft survival, follicle numbers, hormonal restoration, and angiogenesis, likely through eNOS/NO signaling. These scaffolds show good biocompatibility in vivo and integrate with ovarian tissue, supporting cell migration and microvascular network formation. The approach provides a promising strategy for female fertility preservation via ovarian tissue transplantation and suggests a generalizable platform to support transplantation of other organs. Future research should elucidate detailed mechanisms of cell–scaffold interactions (e.g., granulosa cell patterning) and further optimize scaffold composition and long-term in vivo performance.
The study does not fully elucidate the specific mechanisms underlying granulosa cell organization on the scaffold and the precise molecular pathways beyond p-eNOS/NO involved in the pro-angiogenic effect, which the authors note require further investigation. Explicit long-term outcomes beyond the reported time points and broader translational assessments were not detailed.
Related Publications
Explore these studies to deepen your understanding of the subject.