Medicine and Health
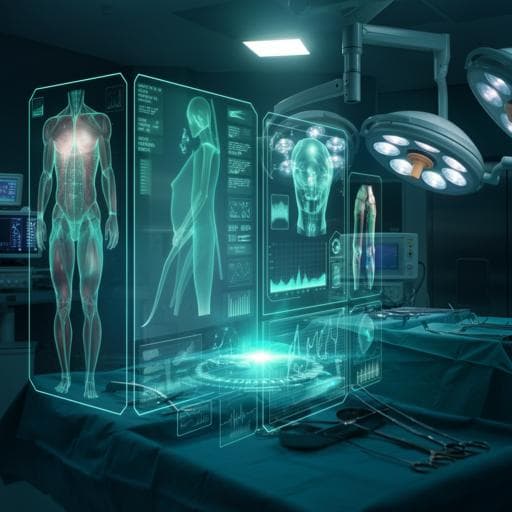
Impact of data on generalization of AI for surgical intelligence applications
O. Bar, D. Neimark, et al.
This study explores how data volume influences AI's ability to generalize in surgical applications. Researchers developed a deep learning system using a diverse cholecystectomy video dataset, achieving impressive accuracy and demonstrating robustness across different medical settings. This work emphasizes the critical role of large datasets for advancing AI in surgery, conducted by Omri Bar, Daniel Neimark, Maya Zohar, Gregory D. Hager, Ross Girshick, Gerald M. Fried, Tamir Wolf, and Dotan Asselmann.
~3 min • Beginner • English
Related Publications
Explore these studies to deepen your understanding of the subject.







