Medicine and Health
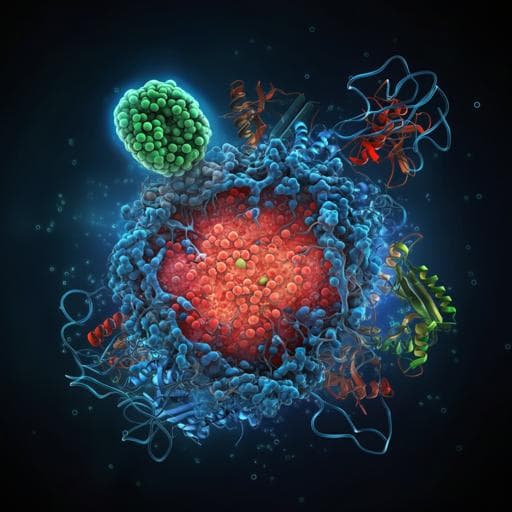
Hsc70 promotes anti-tumor immunity by targeting PD-L1 for lysosomal degradation
X. Xu, T. Xie, et al.
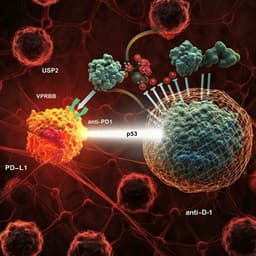
Cancer immune evasion involves suppression and dysfunction of anti-tumor immunity. While PD-1/PD-L1 immune checkpoint inhibition (ICI) has transformed treatment for several cancers, many patients develop primary or acquired resistance. After anti-PD-L1 antibody binding, PD-L1 undergoes internalization; a fraction is degraded in lysosomes, but most is stored in recycling endosomes and returns to the plasma membrane, contributing to ICI resistance. Promoting lysosomal degradation and inhibiting recycling of PD-L1 may overcome resistance. CMTM6, a broadly expressed protein, maintains PD-L1 on the membrane by facilitating its recycling; CMTM6 depletion promotes lysosomal PD-L1 degradation. However, the mechanisms controlling PD-L1 lysosomal degradation remain unclear. Hsc70 (HSPA8) is a cytosolic chaperone pivotal in chaperone-mediated autophagy (CMA) and endosomal microautophagy (eMI). Approximately 40% of mammalian proteins harbor KFERQ-like motifs that can be recognized by Hsc70. Hsc70 can deliver cargo to lysosomes via CMA through Lamp2a or mediate cytosolic cargo internalization into endosomes via eMI by binding phosphatidylserine through its C-terminal lid domain. Substrate routing between CMA and eMI can be determined by protein state and post-translational modifications. Research on PD-L1 degradation has focused mainly on proteasomal pathways, with limited understanding of endosomal-lysosomal routes. This study identifies Hsc70 as a major PD-L1 interactor and investigates its role in PD-L1 degradation via endosome-lysosome pathways and the implications for anti-tumor immunity and ICI therapy.
- Identification of PD-L1 interactors: PD-L1 was immunoprecipitated from HEK293T cells and analyzed by LC-MS/MS to identify interacting proteins. Candidate interactors were assessed for clinical relevance via Kaplan-Meier analysis in breast cancer cohorts.
- Gain- and loss-of-function studies: Hsc70 was overexpressed in MCF-7 and PANC1 cells. PD-L1 mRNA was measured by qRT-PCR; total and surface PD-L1 protein were assessed by immunoblotting and flow cytometry, respectively. Exogenous PD-L1 was also expressed to evaluate Hsc70 effects.
- Pathway dissection of degradation: Pharmacological inhibitors were applied: lysosomal inhibitors (NH4Cl + Leupeptin, E64D), proteasome inhibitor (MG132), macroautophagy inhibitor (3-MA). CMA involvement was tested by manipulating Lamp2a (overexpression/siRNA) and pharmacologically inducing CMA (Spautin-1 + AC220) and monitoring HK2 degradation as a control.
- eMI interrogation: eMI components were perturbed using siRNAs against TSG101 (ESCRT-I) and VPS4 (ESCRT-III ATPase). U18666A was used to disrupt MVB dynamics/eMI. A phosphatidylserine-binding defective mutant Hsc70-3KA was used to test dependency on phosphatidylserine interaction.
- Subcellular trafficking analyses: Confocal immunofluorescence co-localization of PD-L1 with markers of late endosomes (RAB7A), lysosomes (LAMP1), and recycling endosomes (RAB11) following Hsc70-WT or Hsc70-3KA expression and following AUY-922 treatment.
- CMTM6 competition assays: siRNA knockdown of CMTM6 with/without Hsc70 knockdown to assess dependency; co-immunoprecipitation to measure Hsc70–PD-L1 interaction in CMTM6-depleted cells; mapping of Hsc70 binding region on PD-L1 using PD-L1 truncation mutants; testing whether CMTM6 knockdown-mediated PD-L1 degradation depends on eMI (TSG101/VPS4 knockdown, U18666A treatment, co-localization studies).
- Identification and validation of additional mediators: Comparative mass spectrometry of Hsc70-WT vs Hsc70-3KA interactomes to identify enriched pathways/proteins; focus on COPII pathway and TFG. Co-immunoprecipitation of TFG with Hsc70 variants; TFG overexpression/knockdown to assess effects on PD-L1 degradation, surface levels, and organelle co-localization.
- Small-molecule modulation: Treatment with Hsp90 inhibitor AUY-922; time-course assessment of PD-L1 and Hsc70 by immunoblotting; dependence on Hsc70 (siRNA), lysosome/proteasome/macroautophagy inhibitors, CMA (Lamp2a knockdown), and eMI (TSG101/VPS4 knockdown, U18666A). Confocal co-localization with RAB7A, LAMP1, RAB11.
- In vivo studies: Generation of 4T1 murine breast cancer cell lines stably overexpressing Hsc70-WT or Hsc70-3KA, or with PD-L1 knockdown ± Hsc70 overexpression. Orthotopic implantation into female BALB/c (immunocompetent) and BALB/c-nude (immunodeficient) mice. Tumor growth monitoring (volume, weight). Flow cytometry of tumor-infiltrating lymphocytes (CD8+ and GzmB+ CD8+ T cells). IHC for CD8 and GzmB. Tumor cell immunoblotting for PD-L1 and Hsc70. Pharmacologic studies with AUY-922 (i.p. 15–20 mg/kg) ± anti-PD-L1 (100 µg) or anti-CTLA4 (75 µg) in 4T1 models; analyses as above.
- Statistics: One-way or two-way ANOVA with Tukey’s multiple comparisons; t-tests where appropriate; data shown as Mean ± SEM; replicate numbers provided per experiment.
- Hsc70 is a PD-L1 interactor and reduces PD-L1 protein levels: Overexpression of Hsc70 in MCF-7 and PANC1 cells decreased total and surface PD-L1 without altering PD-L1 mRNA, indicating post-transcriptional regulation.
- Degradation is lysosome-dependent, not proteasomal or macroautophagic: Lysosome inhibitors (NH4Cl + Leupeptin, E64D) rescued PD-L1 levels under Hsc70 overexpression; MG132 or 3-MA did not. Manipulating CMA (Lamp2a overexpression/knockdown; Spautin-1 + AC220) did not affect PD-L1, arguing against CMA involvement.
- Hsc70 promotes PD-L1 degradation via endosomal microautophagy (eMI): Knockdown of eMI regulators TSG101 or VPS4 prevented Hsc70-induced PD-L1 reduction and restored surface PD-L1. U18666A blocked PD-L1 degradation and restored surface PD-L1. An Hsc70 mutant defective in phosphatidylserine binding (3KA) failed to reduce PD-L1. Hsc70-WT increased PD-L1 co-localization with late endosomes (RAB7A) and lysosomes (LAMP1) and decreased co-localization with recycling endosomes (RAB11).
- CMTM6 and Hsc70 competitively bind PD-L1: CMTM6 knockdown decreased PD-L1, but concurrent Hsc70 knockdown restored PD-L1, indicating dependency. CMTM6 depletion enhanced Hsc70–PD-L1 interaction. Hsc70’s main PD-L1 binding region mapped to aa 161–241, overlapping with CMTM6’s binding site. The PD-L1 decrease upon CMTM6 knockdown was reversed by TSG101/VPS4 knockdown or U18666A and showed increased PD-L1 co-localization with RAB7A/LAMP1 and decreased with RAB11; Hsc70 knockdown abrogated these effects.
- TFG participates in Hsc70-mediated PD-L1 degradation: Mass spectrometry comparing Hsc70-WT vs 3KA interactors highlighted COPII pathway proteins, with TFG enriched in Hsc70-WT interactome and among top PD-L1 interactors. TFG bound Hsc70-WT more strongly than 3KA. TFG overexpression promoted PD-L1 degradation, while TFG knockdown blocked Hsc70-induced PD-L1 degradation, increased surface PD-L1, and reduced PD-L1 co-localization with RAB7A and LAMP1.
- AUY-922 (Hsp90 inhibitor) induces Hsc70 and drives PD-L1 eMI degradation: AUY-922 reduced PD-L1 and increased Hsc70 protein levels in multiple cell lines. Hsc70 knockdown prevented AUY-922-induced PD-L1 degradation and increased surface PD-L1. Lysosomal, but not proteasomal or macroautophagy inhibition, rescued PD-L1. AUY-922 effects were Lamp2a-independent (non-CMA). TSG101/VPS4 knockdown or U18666A blocked AUY-922-induced PD-L1 degradation and restored surface PD-L1. AUY-922 increased PD-L1 co-localization with RAB7A/LAMP1 and decreased with RAB11.
- In vivo anti-tumor immunity: Hsc70-WT overexpression in 4T1 tumors suppressed growth in immunocompetent BALB/c but not nude mice and increased intratumoral CD8+ and GzmB+ CD8+ T cells; tumor PD-L1 levels were reduced. PD-L1 knockdown or Hsc70 overexpression each suppressed tumor growth and increased CD8 immunity; combining both did not add benefit, suggesting a shared mechanism via PD-L1.
- AUY-922 in vivo efficacy and synergy with ICI: AUY-922 reduced tumor growth in immunocompetent mice, increased CD8+ and GzmB+ T cells, reduced PD-L1, and increased Hsc70 in tumors; no effect in nude mice. AUY-922 combined with anti-PD-L1 or anti-CTLA4 further decreased tumor growth and enhanced intratumoral CD8+ and GzmB+ T cells compared to monotherapy, while reducing tumor PD-L1 and increasing Hsc70. Reported effects were statistically significant (e.g., multiple comparisons with P<0.05 to P<0.0001).
The study addresses resistance to PD-1/PD-L1 ICI that arises from antibody-induced internalization and recycling of PD-L1 back to the plasma membrane. It establishes Hsc70 as a key regulator that redirects PD-L1 toward endosomal-lysosomal degradation through eMI, thereby reducing recycling and surface re-expression. Mechanistically, Hsc70 competes with CMTM6 for PD-L1 binding at an overlapping region (aa 161–241). Loss of CMTM6 increases Hsc70–PD-L1 interaction and drives eMI-dependent PD-L1 degradation. TFG, a COPII/coats-associated protein with roles in endomembrane trafficking, also contributes to this degradative routing. These mechanisms translate into enhanced anti-tumor immunity in vivo, with increased CD8+ T-cell infiltration and activation and reduced tumor growth. Pharmacologically, the Hsp90 inhibitor AUY-922 augments Hsc70 levels and phenocopies Hsc70 overexpression by promoting PD-L1 eMI degradation, improving anti-tumor immunity, and enhancing the efficacy of anti-PD-L1 and anti-CTLA4 therapies. Together, targeting the Hsc70–PD-L1 axis and eMI offers a strategy to limit PD-L1 recycling, overcome resistance to ICI, and potentiate T-cell-mediated tumor clearance.
This work identifies a mechanism whereby Hsc70 promotes PD-L1 degradation via endosomal microautophagy, reducing its recycling to the plasma membrane. Hsc70 competes with CMTM6 for PD-L1 binding, and the trafficking factor TFG facilitates this degradative pathway. Elevating Hsc70—genetically or pharmacologically with the Hsp90 inhibitor AUY-922—decreases PD-L1, enhances intratumoral CD8+ T-cell responses, suppresses tumor growth in immunocompetent mice, and synergizes with anti-PD-L1 and anti-CTLA4 checkpoint blockade. These findings reveal Hsc70-mediated eMI of PD-L1 as a therapeutic target to improve immunotherapy outcomes. Future research should delineate the detailed role of TFG and other trafficking components in PD-L1 eMI, explore modulation of Hsc70 levels or post-translational modifications, and evaluate inhibitors of CMTM6 or regulators of eMI in combination with ICIs across tumor types.
- The precise molecular steps by which TFG and associated trafficking machinery facilitate PD-L1 delivery to late endosomes and lysosomes remain undefined and are highlighted as future investigation.
- While AUY-922 elevates Hsc70 and promotes PD-L1 degradation, endogenous Hsc70 is abundant and stable, posing challenges for direct therapeutic modulation; the study does not fully resolve optimal translational strategies to modulate Hsc70 in patients.
- Most mechanistic experiments were conducted in cell lines and syngeneic mouse models; validation in additional tumor models and clinical contexts is needed to generalize the findings.
Related Publications
Explore these studies to deepen your understanding of the subject.