Medicine and Health
Histones released by NETosis enhance the infectivity of SARS-CoV-2 by bridging the spike protein subunit 2 and sialic acid on host cells
W. Hong, J. Yang, et al.
This groundbreaking research reveals how neutrophil extracellular traps (NETs) in antiviral defense may not be what they seem. Instead of combating SARS-CoV-2, the histones released during NETosis actually boost the virus's infectivity. Conducted by a team of experts including Weiqi Hong and Jingyun Yang, this study opens new pathways for COVID-19 therapies.
~3 min • Beginner • English
Introduction
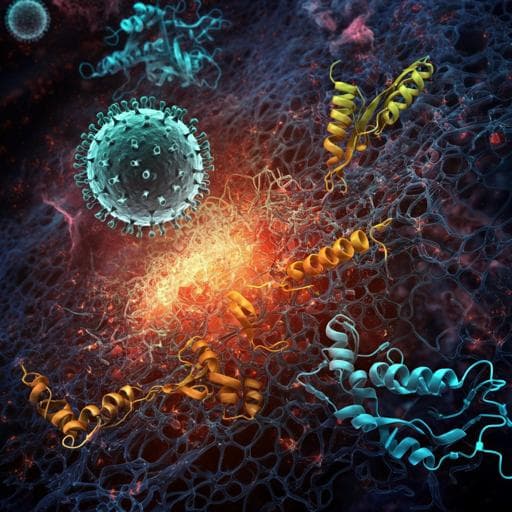
The study investigates whether neutrophil extracellular trap (NET) formation (NETosis) influences SARS-CoV-2 infectivity and explores mechanisms beyond ACE2-mediated entry. While S1 of the SARS-CoV-2 spike protein is known to bind ACE2 and several coreceptors (neuropilin-1, heparan sulfate, SR-B1, AXL, CD147), it was unclear whether S2 interacts with host factors. The authors hypothesize that positively charged histones released during NETosis might bridge the negatively charged S2 subunit to negatively charged molecules on host cells, such as sialic acid, thereby enhancing viral attachment, membrane fusion, and infectivity. The purpose is to elucidate this potential mechanism using live virus, pseudovirus systems, biochemical binding analyses, and an in vivo mouse model.
Literature Review
Background knowledge highlights that NETs can capture and inactivate viruses (influenza, HIV, RSV) via chromatin backbones and antimicrobial components (e.g., MPO, α-defensin). Histones, abundant in NETs and positively charged, can exert antiviral effects and NET components can activate immune cells. However, excessive NETs cause tissue damage; extracellular histones are cytotoxic and implicated in thrombosis, with polysialic acid mitigating cytotoxicity. Elevated NETs and histones have been reported in severe COVID-19 samples, and SARS-CoV-2 can trigger NETosis. Prior studies identified multiple S1-associated host factors (neuropilin-1, heparan sulfate, SR-B1, AXL, CD147), but no host factor was reported to interact with S2. This context motivates examining whether NET-derived histones influence SARS-CoV-2 infectivity via S2 and host cell glycans like sialic acid.
Methodology
- Virus and cell systems: Used live SARS-CoV-2 to infect Vero E6 cells and lentiviral pseudoviruses bearing SARS-CoV-2 spike (EGFP or luciferase reporters) to infect HEK-293T cells expressing ACE2 (293T/ACE2) and Calu-3 lung epithelial cells. Infection readouts included cytopathic effect (CPE), EGFP positivity (flow cytometry, microscopy), and luciferase activity.
- NETosis manipulation: Human neutrophils were incubated with SARS-CoV-2 or pseudovirus in the presence or absence of PMA (10–100 nM) to induce NETosis. Cl-amidine (PAD4 inhibitor, 50–200 µM) was used to inhibit NETosis. Supernatants were collected and applied to target cells. DNase I was tested to assess DNA contribution.
- Histone treatments and blocking: Pseudovirus or live virus was preincubated with total histones or purified histones H2A, H2B, H3, H4 (0.5–25 µg/ml; most experiments at 0.5–5 µg/ml) at 37 °C for 3 h before infection. Blocking antibodies against H3 or H4 (10 µg/ml) and isotype controls were used to neutralize histone effects.
- Binding assays: ELISA-like binding assays coated plates with histone H3 or H4 (1 µg/ml) and tested binding of biotinylated spike ectodomain (S1+S2), S1, S2, RBD, or ACE2 (0–100 nM). Detection was via streptavidin-HRP at 450 nm.
- Surface plasmon resonance (Biacore 8K): Immobilized H3 or H4 on CM5 chips (~25 RU). Analytes (S1+S2, S1, S2; 78–1250 nM) in HBS-EP+ buffer; association/dissociation monitored; KD values calculated. Sensor regeneration with glycine pH 1.5.
- Computational modeling: ZDOCK for rigid-body docking using S trimer (PDB 6VSB) and histone (PDB 6HKT), with ZRANK rescoring and clustering; clashes with N-glycans filtered. Electrostatic potential mapping of S2 C-terminus. Molecular dynamics (NAMD) with CHARMM36 and CGenFF to estimate interaction energies and per-residue contributions; modeling included histone interactions with S2 and sialic acid (PDB 2CWG).
- Spike mutagenesis: Two mutants targeting acidic S2 C-terminal submotifs were generated by Gibson Assembly: Mut-1 (D1139P, E1144K, E1150S, D1153S) and Mut-2 (D1163A, D1165N, D1168S, D1184N, E1188Q, E1195N, D1199N). Corresponding pseudoviruses were produced.
- Sialic acid/heparan sulfate perturbations: Cells pretreated with neuraminidase (NA; 0.1 U/ml) or heparin lyases I/II/III (HSase) to remove surface sialic acids or heparan sulfate. Histones were preincubated with free sialic acid (Neu5Ac; 10 µg/ml) or polysialic acid (PSA; 10 µg/ml) for competition.
- Cell binding assays: Flow cytometry with biotin-tagged H3 or H4 to measure binding to Calu-3 cells, with/without NA or Neu5Ac. Biotin-tagged S2 preincubated with H3 or H4 to assess S2-histone complex binding to cells and its sensitivity to NA.
- Cell-cell fusion: Co-culture of 293T cells expressing SARS-CoV-2 S (C-terminal 18-aa truncation) and EGFP with 293T/ACE2 target cells, ± H3 (1 µg/ml) or H4 (2 µg/ml). NA pretreatment of effector or target cells assessed sialic acid dependence. Syncytia quantified microscopically.
- Mouse model: hACE2-transgenic C57BL/6 mice received intratracheal instillation of SARS-CoV-2 (4×10^5 PFU in 60 µl). In some groups, virus was preincubated 3 h at 37 °C with total histone, H3 or H4 before instillation. Separate groups received daily intraperitoneal Cl-amidine (50 mg/kg) or Neu5Ac (20 mg/kg) immediately post-challenge for 5 days. Lungs collected day 5 for analyses.
- In vivo assays: Confocal immunofluorescence for NETosis markers (MPO, histone H3) and spike localization; RT-qPCR for subgenomic E sgRNA; TUNEL assay for apoptosis quantification.
Key Findings
- NETosis enhances infectivity: Supernatants from PMA-activated neutrophils increased infectivity of live SARS-CoV-2 in Vero E6 cells compared to unactivated neutrophils; effect was abolished by Cl-amidine (PAD4 inhibitor). DNase I did not reduce pseudovirus enhancement, suggesting DNA in NETs is not the driver.
- Histones H3/H4 promote infection: Preincubation of pseudovirus with total histone, H3, or H4 increased infection in 293T/ACE2 and Calu-3 cells; H2A/H2B had weaker effects and required higher concentrations. H3/H4 also enhanced infectivity of live SARS-CoV-2; histones alone were not cytotoxic at tested doses. Anti-H3 or anti-H4 antibodies blocked the enhancement.
- Selective binding to S2: ELISA-like assays showed stronger binding of S2 or S ectodomain to immobilized H3/H4 than S1, RBD, or ACE2. SPR KDs (µM): H3–S2 0.05, H3–S (S1+S2) 0.44, H3–S1 >3.70; H4–S2 0.04, H4–S (S1+S2) 0.22, H4–S1 >3.30, indicating selective high-affinity interaction with S2.
- Computational support and key residues: Docking/MD identified an electronegative surface at S2 C-terminus engaging histones. Calculated interaction energies: H3–S about −579.6 kcal/mol, H4–S about −665.3 kcal/mol. Residues D1139, E1144, E1150, D1153 contributed strongly; S1147 and F1148 supported via hydrogen/hydrophobic interactions. Mut-1 (D1139P/E1144K/E1150S/D1153S) reduced histone-mediated enhancement; Mut-2 (D1163A/D1165N/D1168S/D1184N/E1188Q/E1195N/D1199N) had no effect.
- Sialic acid is the host-side bridge: Modeling suggested multivalent interactions between histones and sialic acid; reported energies for histone–sialic acid interactions were −505.6 kcal/mol (H3) and 600.4 kcal/mol (H4). Flow cytometry showed H3/H4 binding to Calu-3 cells was reduced by neuraminidase (NA) pretreatment or by preincubating histones with free sialic acid. S2 alone bound poorly to cells, but S2–histone complexes bound efficiently; NA blocked this binding.
- Functional dependence on sialic acid: Histone-enhanced pseudovirus infectivity was inhibited by NA, free Neu5Ac, or polysialic acid (PSA). Heparin lyase treatment reduced baseline pseudovirus infectivity but did not diminish histone-mediated enhancement, indicating a pathway distinct from S1–heparan sulfate interaction.
- Enhanced membrane fusion: H3 and H4 increased S-mediated cell–cell fusion (syncytia). NA pretreatment of ACE2-expressing target cells, but not S-expressing effector cells, abrogated histone-enhanced fusion. NA alone had no effect without histones.
- In vivo evidence: In SARS-CoV-2–infected hACE2 mice, neutrophil NETosis was observed in lungs, with extracellular histone debris colocalizing with spike-positive particles. Treatments with Cl-amidine or Neu5Ac significantly reduced lung sgRNA loads and TUNEL-positive apoptotic cells. Conversely, preincubating virus with total histone, H3, or H4 increased lung sgRNA levels and apoptosis.
Discussion
Findings reveal that SARS-CoV-2 can exploit NETosis-derived histones, particularly H3 and H4, to enhance host attachment and entry by bridging the negatively charged S2 C-terminal domain to sialic acids on host cell surfaces. This mechanism is distinct from previously characterized S1 interactions (e.g., heparan sulfate) and identifies, for the first time, a host factor-mediated facilitation via S2. The biochemical, biophysical, computational, and mutational data converge on a specific acidic patch (D1139, E1144, E1150, D1153) as a histone interaction hotspot. Functionally, this bridging augments both virion entry and S-mediated cell–cell fusion and is sialic acid dependent. In vivo, modulating NETosis (with Cl-amidine) or competing for histone binding (Neu5Ac) mitigated viral replication and tissue apoptosis, while exogenous histones exacerbated disease markers. These results suggest therapeutic avenues targeting NETosis, neutralizing extracellular histones, or blocking histone–S2 or histone–sialic acid interactions to reduce SARS-CoV-2 infectivity and pathology.
Conclusion
The study demonstrates that extracellular histones released during NETosis, especially histones H3 and H4, bind selectively to the S2 subunit of the SARS-CoV-2 spike protein and bridge it to sialic acids on host cells, enhancing viral attachment, membrane fusion, and infectivity. Evidence spans live virus and pseudovirus assays, binding and SPR measurements, computational modeling, targeted spike mutagenesis, and an hACE2 mouse model. Therapeutically, inhibiting NETosis (e.g., PAD4 inhibition), neutralizing extracellular histones, or blocking histone–S2/sialic acid interactions may reduce SARS-CoV-2 infection and lung injury. Future work should validate these mechanisms across variants, quantify histone levels and sialylation states in patient tissues, and develop targeted inhibitors or decoys to disrupt this bridging pathway.
Limitations
Related Publications
Explore these studies to deepen your understanding of the subject.