Medicine and Health
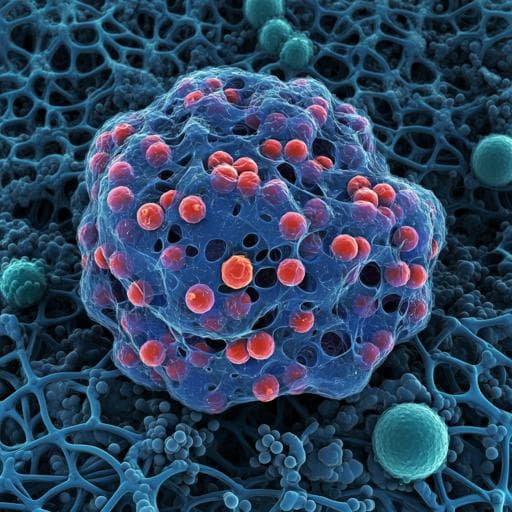
Highly porous and injectable hydrogels derived from cartilage acellularized matrix exhibit reduction and NIR light dual-responsive drug release properties for application in antitumor therapy
M. Gulfam, S. Jo, et al.
Discover groundbreaking research by Muhammad Gulfam and colleagues on innovative injectable hydrogels that respond to stimuli. These hydrogels, created using biocompatible cartilage acellularized matrix and cutting-edge click chemistry, enable precise drug delivery and targeted treatment. With impressive mechanical properties and minimal drug release under normal conditions, they offer potential breakthroughs in cancer therapy through NIR light activation.
Related Publications
Explore these studies to deepen your understanding of the subject.