Medicine and Health
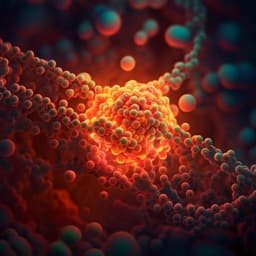
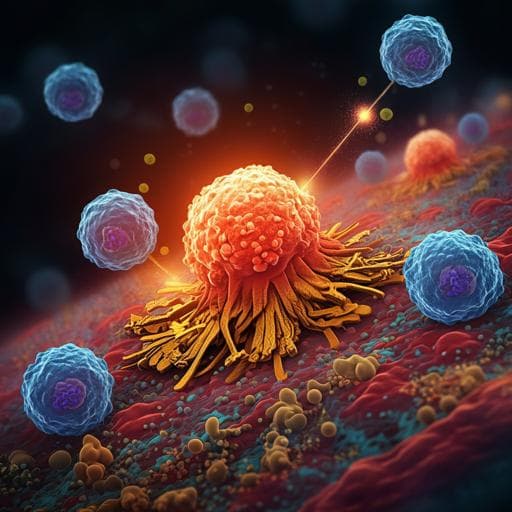
Fractionated photoimmunotherapy stimulates an anti-tumour immune response: an integrated mathematical and in vitro study
M. U. Zahid, M. Waguespack, et al.
This research, conducted by Mohammad U. Zahid and colleagues, explores innovative approaches to combat advanced epithelial ovarian cancer (EOC) through mathematical modeling of tumor-immune interactions. By integrating in vitro measurements, they reveal how fractionated photodynamic therapy (PIT) can enhance anti-tumor immune responses, presenting a promising avenue for optimizing cancer treatment.
Related Publications
Explore these studies to deepen your understanding of the subject.